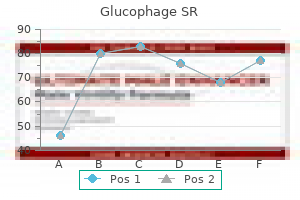
Glucophage SR
Buy glucophage sr 500mg
Applicability and relevance of models that predict short term outcome after intracerebral haemorrhage medicine 911 cheap 500mg glucophage sr visa. Prognostic Tools for Early Mortality in Hemorrhagic Stroke: Systematic Review and Meta-Analysis. Clinician judgment vs formal scales for predicting intracerebral hemorrhage outcomes. Early care limitations independently predict mortality after intracerebral hemorrhage. Variability in physician prognosis and recommendations after intracerebral hemorrhage. Predicting mortality in spontaneous intracerebral hemorrhage: can modification to original score improve the prediction? Multiplicity of risk factors in ischemic stroke patients: relations to age, sex, and subtype-a study of 2,505 patients from the lund stroke register. Comparison of the Glasgow Coma Scale and the Reaction Level Scale for assessment of cerebral responsiveness in the critically ill. Reliability of intracerebral hemorrhage classification systems: A systematic review. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Editorial comment-Stroke incidence studies one step closer to the elusive gold standard? Leukoaraiosis on magnetic resonance imaging correlates with worse outcomes after spontaneous intracerebral hemorrhage. Long term (13 years) prognosis after primary intracerebral haemorrhage: a prospective population based study of long term mortality, prognostic factors and causes of death. Intraventricular extension of supratentorial intracerebral hemorrhage: the modified Graeb scale Improves outcome prediction in Lund Stroke Register. Applicability of clinical trials in an unselected cohort of patients with intracerebral hemorrhage. Copyright © 2016 Wolters Kluwer Health Lippincott Williams & Wilkins stroke. However, all current treatment modalities are far from perfect and are associated with serious tively and therefore are osmotically the most active). From the Department of Neurology and Neurosurgery, Uni It is important to point out that different types of versity Hospitals of Cleveland and Case Western Reserve University, Cleveland, Ohio. For instance, brain ischemia is associated with both cytotoxic and Address: Jose´ I. Small increases through normalization of intracellular sodium and 13 in brain volume can be compensated by changes in chloride concentrations. The autoreg longer duration of action and to yield greater 13 ulatory mechanisms of the brain vasculature have improvement in cerebral perfusion pressure. It has been postulated, Some of the published studies are briefly reviewed 13 based on experimental animal data, that increased here. However, the report of 2 patients with nontraumatic (presumably administered solutions used were not equiosmolar. Suarez et al retrospectively In a retrospective review of 8 patients with studied 29 patients with symptomatic vasospasm intracranial hypertension refractory to hyperventi 36 and hyponatremia who received continuous infu lation, mannitol, and furosemide, Suarez et al sions of 3% saline. The authors demonstrat sure with a subsequent increase in cerebral perfusion ed an increase in cerebral perfusion pressure and a pressure. Malignant cerebral edema and intracra venous congestion; intracerebral, subdural, and nial hypertension. Comparisons of mannitol regimens in patients with severe head injury undergoing tical vein thrombosis with hemorrhagic infarction. The University of 6 Toronto head injury treatment study: a prospective, randomized found to cause similar changes in animal models. Cerebrospinal Fluid in Diseases of the venous infusions, but it is followed by an elevation Nervous System. Cerebral blood times have been reported with large-volume infu flow is regulated by changes in blood pressure and blood viscosity 43 alike. Renal failure was reported to occur with saline attenuates microcirculatory disturbances after traumatic 44 brain injury. There are several possible mechanisms of not improve cerebral oxygen delivery after head injury and mild action, and important complications such as central hemorrhage in cats. Effects pontine myelinolysis and intracranial hemorrhage of hypertonic saline hydroxyethyl starch solution and mannitol in have not been reported in the human studies. Effects of ods of infusion (bolus and continuous) have been hypertonic (10%) saline in patients with raised intracranial pres used in the past, and so far there are not enough sure after stroke. Malignant cerebral edema in patients with hypertensive intracerebral hemorrhage associated er. Many issues remain to be clarified, including the with hypertonic saline infusion: a rebound phenomenon? Administration of ic solutes (sodium chloride or mannitol) in the treatment of hypertonic (3%) sodium chloride/acetate in hyponatremic refractory posttraumatic intracranial hypertension: 2 mL/kg 7. J Neurosurg 1988; versus 20% mannitol during elective neurosurgical supratentorial 68:478–481. Use of hypertonic cotic hydroxyethyl starch decreases intracranial pressure follow (3%) saline/acetate infusion in the treatment of cerebral edema: ing neurotrauma. Is there a therapeutic role for osmotic breaching of of intracranial hypertension. Hypertonic saline worsens saline resuscitation of patients with head injury: a prospective, infarct volume after transient focal ischemia in rats. Osmotic demyelination syn tive, randomized and controlled study of fluid management in drome following correction of hyponatremia. N Engl J Med 1986; children with severe head injury: lactated Ringer’s solution versus 314:1535–1542. Anesth acetate infusion in treatment of cerebral edema in patients with head Analg 1991; 73:597–602. J Trauma in the treatment of severe refractory posttraumatic intracranial 1991; 31:8–14. Centers for Disease Control and Prevention National Center for Injury Prevention and Control Thomas R. Director, Centers for Disease Control and Prevention National Institutes of Health National Institute of Neurological Disorders and Stroke National Center for Medical Rehabilitation Research, Eunice Kennedy Shriver National Institute of Child Health and Human Development Francis S. Director, National Institutes of Health the inclusion of individuals, programs, or organizations in this report does not constitute endorsement by the U. Report to Congress on Traumatic Brain Injury in the United States: Understanding the Public Health Problem among Current and Former Military Personnel. Director, Centers for Disease Control and Prevention Administrator, Agency for Toxic Substances and Disease Registry Department of Health and Human Services Francis S. Epidemiologic and clinical studies suggest that many of these military service-related injuries have serious long-term health and socioeconomic consequences. This report represents the culmination of the Leadership Panel’s deliberations and summarizes findings and recommendations. Deputy Director National Institute of Neurological Disorders and Stroke National Institutes of Health Building 31, Room 8A52 31 Center Dr. Scientific Program Manager for Brain Injury Rehabilitation Research and Development Service Office of Research and Development U. It was developed through a collaborative effort of a Leadership Panel made up of representatives from the four participating agencies/departments and was reviewed, cleared, and approved by the participating agencies/departments. All four participating agencies should continue to foster and strengthen collaboration to this aim. Update these definitions periodically as more precise, sensitive, and valid terms and definitions are available. More details on each of the recommendations, including the rationale and potential benefits, can be found in this document. These forces might temporarily or permanently disrupt the functioning of the brain. The use of protective gear can reduce the occurrence and severity of brain injuries. Multiple severe concussive and sub-concussive injuries, like those reported in boxers who engaged in the sport for several years, are known to cause a delayed dementia syndrome (dementia pugilistica or chronic traumatic encephalopathy) (Zetterberg et al. For example, a blow to the head from a fall can cause bleeding and bruising of the brain.
Buy generic glucophage sr 500 mg line
It features the large nuclei known as the paired inferior olivary nucleus (this is what accounts for the outward bulging seen superficially as the inferior olive) symptoms zoloft overdose order glucophage sr without a prescription. This nucleus is part of an extensive group of brainstem nuclei that project to the cerebellum. A prominent fiber bundle on the lateral surface of the medulla is the incipient inferior cerebellar peduncle (not yet attached to the cerebellum at this point). You can see that the tegmentum of the medulla contains many different cell groups. With reference to Figures 4 & 5 and the chart below, carefully inspect the internal features of the medulla from its caudal union with the spinal cord to the pons. Spend some time browsing these medullary sections (and the sections in Sylvius4 Online), and find each of the internal features described in the chart below. The caudal and middle pons (upper and lower sections, respectively; “7-pons” & “6-pons” in Sylvius4 Online) look very similar at first inspection. We need two levels to represent the pons because there are different groups of cranial nerve nuclei at the two levels. These sections are attached to the cerebellum (a dead giveaway that we are in the pons) by the massive middle cerebellar peduncles (cut on the lateral edge of the sections). The base of the pons is made up of a mix of cells—the pontine gray matter and transversely coursing fibers—fibers that arise from the cells in the pontine gray matter and travel into the cerebellum via the middle cerebellar peduncle. The tegmentum of the pons looks similar at both levels, but the nuclei contained at each level are different. Pons With reference to Figures 6 & 7 and the chart below, carefully inspect the internal features of the pons. Spend some time browsing these pontine sections (and the sections in Sylvius4 Online), and find each of the internal features described in the chart below. The fourth ventricle, which you saw in the sections through the pons, is disappearing to be replaced by the cerebral aqueduct. It terminates in a superficial nucleus of the dorsal-lateral upper medulla called the cochlear nucleus. Although not labeled in Sylvius4, it is visible in the section labeled “8-Medulla” as the gray matter that wraps around the dorsal-lateral surface of the inferior cerebellar peduncle 12 Internal Anatomy of the Brainstem Midbrain With reference to Figures 8 & 9 and the chart below, carefully inspect the internal features of the midbrain. Superior colliculus Medial geniculate Cerebral nucleus (part of aqueduct the thalamus) Lateral geniculate nucleus (part of the thalamus) Cerebral peduncle Substantia nigra Red nucleus Figure 8. This section is through the rostral midbrain and so it cuts through the superior colliculus. These are the substantia nigra and the red nucleus; they are discussed in a later session. The last section in the series through the brainstem is cut through the junction of the midbrain and diencephalon. Structures of the midbrain are seen medially, but laterally the diencephalon has appeared. The cerebral peduncles will become continuous with the internal capsule a little rostral to this level. Note the presence of the subthalamic nucleus on the dorsal aspect of the cerebral peduncle (in the place where the substantia nigra is located a centimeter inferior to this level; cf. In conclusion, multimodal neuroradiological images are very useful for invasive non circumscribed brain tumors such as glioma and, in combination with such highly technological analyses, advanced neurosurgical procedures are possible. As a result, it is becoming possible to establish a correct diagnosis of a minute lesion. In a neurosurgical operation, this information integration among image, organ and function assures a good balance between maximum tumor resection for overall survival prognosis and provides a functional prognosis even for invasive malignant brain tumors4). Furthermore, this innovation provides the momentum for development of surgical devices applicable even in the microscopic feld5). At present, the Department of Neurosurgery, Nagoya University Graduate School of Medicine is working on a project for “development of an intelligent operation system” along with the Department of Mechanical Engineering, Nagoya Institute of Technology and Department of Media Science, Nagoya University Graduate School of Technology. The goal of the project is to create the world’s frst intraoperative brain touch sensor and/or microsurgical device for microscopic or endoscopic management. Additionally, by making this available on line, it is possible to share the surgical assist Fig. With the great technical assistance of the Graduate School of Information Science, Nagoya University and the Department of Radiological Technology, Nagoya University School of Health Science, the system can develop educational and training activities for students and young neurosurgeons in terms of surgical simulation before an operation. Besides, the simulated experience of operations produced by sharing virtual images is useful to decide the strategy for clinical cases. Since it is a Nagoya University-affliated hospital, these two systems are linked by network to exchange information so that it is now possible to assist with diffcult operations mutually by remote control. It is easy to imagine that the surgical assist system brought about by 3D virtual images will show rapid progress hand in hand with the advancement of image analysis. Along with advancements in diagnostic radiology, various kinds of neuroimaging are produced which are useful for preoperative diagnosis, planning operation strategy, intraoperative image assistance, and postoperative follow-up. Such evolution foretells the near future when tissue diagnosis can be done merely by image analysis. The use of these various technologies for preoperative evaluation and intraoperative assistance has made more accurate neurosurgery feasible. Moreover, progress in computer technology makes it possible to utilize advanced 3D virtual images for more advanced image analysis. Yu-ichiro Hayashi, PhD) has designed the fastest software for image analysis and collaborative research is expected to deliver optimum results. Meanwhile, it is also obvious that continuous efforts by neurosurgeons have resulted in excellent progress. Brain tumors, particularly in infltrative intraparenchymal tumors such as glioma, require delicate surgery; however, wide tumor resection might cause brain dysfunction and/or an adverse effect. Therefore, an immediate decision based on both improved resection and avoidance of dysfunction is necessary. Note remarkable “brain shift” after connection of ventricle with tumor removal cavity. The neuronavigation system is a useful surgical-assisted device which can provide accurate information on the surgical site in real time. However, existing navigation functioned based on preoperative imaging has inherent fundamental problems involving the “brain shift. Since this change in brain shape undermines the reliability of navigation which uses a preoperative image as a map, the appropriate adjustment for such brain shifts has become an urgent necessity. Three kinds of information, image, organ, and function, should be integrated to balance competing goals for maximum resection and ensuring safety (Fig. Present advances in prevention medicine enhance the opportunities for early detection by brain medical checkups and rapid cures of neurosurgical disorders, that might otherwise cause serious disability. Now we are at a major turning point for neurosurgical treatment since safer and more secure ways of providing it have been established as prevention measures in recent years. Now there is a pressing need to create a support system by promoting expertise and innovations to meet the increasing demand for neurosurgical treatment. World’s frst magnetic resonance imaging/X-ray/operating room suite: a signifcant milestone in the improvement of neurosurgical diagnosis and treatment. Accuracy of diffusion tensor magnetic resonance imaging tractography assessed using intraoperative subcortical stimulation mapping and magnetic source imaging. Glioma surgery using a multimodal navigation system with integrated metabolic images. Brain stem: the brainstem is located at the juncture of the cerebrum and the spinal column. But, make sure you know the structures which make up each brain division, the location of each, and a short summary of the function of each structure which is included in the list above (plus its location). Epithalamus: the epithalamus is a dorsal posterior segment of the diencephalon (a segment in the middle of the brain also containing the hypothalamus and the thalamus) which includes the habenula, the stria medullaris and the pineal body. Its function is the connection between the limbic system to other parts of the brain. Some functions of its components include the secretion of melatonin by the pineal gland, and the regulation of hunger and thirst by the habenula.
Diseases
- Schwartz Newark syndrome
- Erb Duchenne palsy
- Susac syndrome
- Short limb dwarf oedema iris coloboma
- Retinal telangiectasia hypogammaglobulinemia
- Hunter Rudd Hoffmann syndrome
Buy glucophage sr now
Furthermore medications covered by blue cross blue shield purchase glucophage sr 500mg with mastercard, the genome instability of neoplasms increases the likelihood of other cells developing skills that allow for the development of metastasis. Several studies have shown that an increase in metastatic ability is not the result of the adaption mechanisms of the tumour cells that allows for growth in a specific organ; rather, it is the gradual selection of a clone with different mutations to those observed in the primary tumour. The genome instability and heterogeneity of cancer cells is shown in the gains, losses, and chromosomal rearrangement of the tumours [11]. New technologies in parallel sequencing have allowed high-resolution genome analysis of cancer patients, making it possible to compare the primary tumour with regard to metastasis. These studies have proven that there are inactive genes in the primary tumour, while they are active in metastasis, allowing for the activa tion of other oncogenes, confirming the concept of tumour heterogeneity [12]. Additionally, it has been shown that mutation patterns are shared in the metastasis of an organ, whereas metastasis in the different organs of a patient is different, establishing the hypothesis that metastasis results from clonal expansion where the subclones that have colonised an organ already have genetic alterations that allow specific adaption to the environment [13]. The period of time that passes between infiltrating the organ and colonising it is known as the latency period, where several tumour cells remain outside the cell cycle of secondary organs, while others are incapable of provoking the angiogenic changes necessary for tumour expansion [14]. It would appear that metastasis is a process determined by a complex network of interactions between metastatic cells and their microenvi ronment in the affected organs, making it necessary to update the contributions made for the knowledge of the different microenvironment elements involved in the formation of metastasis. It is necessary to focus on the main interactions established between the tumour cells and the microenvironment, from the primary tumour to reach the location where metastasis originates and develops. In all these phenomena, time has to also be considered as a factor of singular and paramount importance (Figure 2). In metastatic progression, time and the failure factors indicated in the fgure above, play a crucial role in the prognosis and treatment of the patient with cancer, as shown in the model of the linear progression of a tumor. Thus the concept of ‘metastasis of metastasis’ is used in reference to the metastasis becoming in the course of time more malignant, resulting in the death of the patient, as the illness cannot be controlled. Added to this is the participation of untransformed cells, such as fibroblasts and endothelial cells, as well as the deposition of molecules such as fibronectin, tenascin-c, and periostin [15]. The development and consolidation of these inves tigations originated from the pioneering work made by Kaplan and co. They also studied the adhesion and formation of aggregated cells after the implantation of the tumour cells, observing a growth in the expression of fibronectin and an increase in the dissemination of fibroblasts found in the primary tumour. Likewise, this signalling not only stimulates tumour progression but also induces the production of cytokines by the tumour cells themselves [20]. Neutrophils They are the most abundant human leukocytes as they are the first cells that gather at the infection site. It has been shown that in various types of tumours, they present specific modifications in its stimulating ability with the consequent abnormal development of the differentiation of myeloid cells [27]. When they are immature cells, they seem to have monocyte/macrophage and granulocyte characteristics [33]. Experimental data suggest that these cells are also capable of being different from endothelial cells [35]. T cells the inhibition of the flow of T-lymphocytes during angiogenesis and stroma restructuring represents a characteristic of the tumour microen vironment, giving way to alterations to its functionality. This is due to the activation and expansion of myeloid cells and soluble factors secreted by the tumour and inflammatory cells. In the development of solid tumours with similar characteristics to dam aged tissues with immune dysfunction, such as chronic immune cell infiltration, tissue restructuring or angiogenesis, it is unsurprising that individuals with autoimmune diseases are at increased risk of developing cancer [43]. These data indicate that the activation of B cells is essential for the development of an epithelial neoplasm and that soluble mediators secreted by B cells are necessary to establish an inflammatory process that boosts tumour progression [46]. Mast cells They represent a peculiar subtype of granulocytes that play a central role in the inflammatory process, participating in vascularisation during arthritis [47]. They have also been found to participate in the vascularisation of haematological malignancies, where they can integrate in the blood vessel wall by vascular mimicry [48]. The participation of mast cells in angiogenesis is associated with the production of various cytokines and chemokines [49]. B-triptase is a neutral protease that represents an abundant mediator found next to mast cell granules and plays an important role in inflammation, activating the release of protease by type 2 receptors that are directly involved in vascularisation [51]. Macrophages are typically con sidered as effector cells during immune defence but numerous studies have shown their role in tumour progression [52]. They are an impor tant source of proteases, such as cysteine and cathepsin, that participate in tumour progression [53]. Tumour-associated macrophages have antagonistic functions between the homeostasis of normal tissues and tumorigenesis, which is why macrophages are functionally plastic and can alter their phenotype to suit different physiological conditions [54]. They can present a ‘M1’ phenotype that produces a type 1 pro-inflam matory cytokine that participates in antigen presentation, playing an antitumorigenic role, as well as a ‘M2’ phenotype that produces a type 2 cytokine that promotes the anti-inflammatory response and pro-tumorigenic function [55]. It should be noted that the accumulation of tumour-associated macrophages is linked with angiogenesis and the subsequent acquisition of invasive phenotypes [56]. These blood clots recruit myeloid-derived suppressor cells in secondary niches, impeding the immunological rejection of the tumour [58]. There are numerous cancer associated fibroblasts in the tumour microenvironment, differing from normal fibroblasts. In mice, normal prostrate epithelial cells originate in intraepithelial tumours when coinjected with cancer-associated fibroblasts, but not when they are injected with normal fibroblasts [60]. Likewise, in breast cancer, cancer-associated fibroblasts stimulate the metastasis of malignant cells, while normal fibroblasts suppress metastasis [61]. This shows that cancer-associated fibroblasts make up a cell different to its normal counterpart. Moreover, their origin during the progression of the disease is unclear [62]; several studies suggest that they generate through the epithelial–mesenchymal transition of endothelial cells from blood vessels associated with tumours [63]. Cancer-associated fibroblasts interact with tumour cells and additional components of the stroma through the production and secretion of various growth factors, cytok ines, and chemokines. Pericytes They are specialised mesenchymal cells that are linked to smooth muscle, which act as support to endothelial cells and contribute both towards homoeostasis and the stabilisation, maturation and restructuring of capilliaries [72]. The intimate anatomical relationship between endothelial cells and pericytes suggests a stretched interaction between cell contacts by paracrine signalling. Angiopoietin-1 (Ang-1) is a soluble ligand produced by pericytes that joins with the tyrosine kinase receptor Tie-2, expressed by endothelial cells [74]. The interaction between Ang-1 and Tie-2 is fundamental for the maturation and stabilisation of the endothelium [75]. Vascularisation in tumours is chaotic and irregular, an instability that has been frequently attributed to a reduc tion in the number of pericytes [77]. The presence of pericytes can vary according to the type of tumour, considering that they increase in pancreatic cancer for example and decrease in glioblastoma, a notable fact when compared with the respective normal tissues. In reality, they are found in the majority of tumours, even though their association with the endothelium is abnormal [78]. A hypothesis considers that the reduction of the number of pericytes in tumour vessels can increase intravasation of cancer cells, promoting its haematogenous dissemination [78]. In fact, it has shown the existence of an inverted link between the contents in pericytes of tumour vessels and the number of metastasis in colorectal cancer patients [80]. It is also possible that this occurs through the reduction of the number of dendritic cells, which are essential to initiating and maintaining an antitumour immune response [83]. The T regulator cells (Treg) are found in the tumour microenvironment and have several immunomodulator activities in cancer [89]. In normal physiological conditions, the Treg cells regulate the expansion and activation of the T and B lymphocytes, playing a critical role in the cytotoxic homoeostasis of the lymphocytes [90]. Based on the response to different environmental stimuli, the Treg cells have different effects on tumorigenesis, for example in breast tumours, which show that an increase in Treg cells is correlated with a lower survival [91], while in colorectal cancer, the Treg cells are associated with a higher survival [92]. The S100A8 and S100A9 proteins, produced by primary tumours, induce the accumulation of haematopoietic progenitor cells and macrophages in pre-metastatic regions of the lung. This pro-inflammatory condition accelerates the migration of the primary tumour cells to the pre-metastatic niche in the lung [94]. In an animal model with metastasis in the lung, significant changes were observed in the vascular permeability that contributes to the establishment of the metastasis. The epithelial–mesenchymal transition Local invasion implies profound changes in the adhesion and the proteolytic and migratory properties of the tumour cells, which favours cellular disassociation, degradation of the extracellular matrix, and migration to adjacent tissues. In addition, the excessive proliferation of epithelial cells and angiogenesis are the markers of initiation and growth, which can be observed in a primary carcinoma [96]. During the progression of a carcinoma, the already differentiated tumour cells alter their genome, which confers an advantage on the cell in terms of growth. In later stages, the cells continue to change their genome and exhibit a non-differentiated phenotype frequently accompanied by a low expression of epithelial markers, which leads to a loss of intercellular junctions and epithelial polarity. These changes are often accom panied by an increase in the expression of mesenchymal markers, as well as the mobility of the cells, which gives them greater invasive capacity.
Order glucophage sr online now
A cavernoma in the ventricle is not always limited by the ependyma and can extend to the surrounding brain and we classified cavernomas into three groups medicine valium generic glucophage sr 500mg visa, accordingly. Although our classification is only empirically based, we suppose that in clinical practice the treatment strategy of the cavernomas of group C is quite similar to intraparenchymal ones. In our series, repetitive re-hemorrhages accompanied by acute headaches with nausea and vomiting occurred often and caused discomfort. Four of our nine patients who were operated on had neurological deficits that persisted at follow-up, but in two of these deficits were already present before surgery (Table 18). Patients with cavernomas close to the brain stem frequently present preoperatively with cranial nerve deficits as a sign of brain-stem damage. Therefore, the increased morbidity in our series may be explained by our rather short follow-up and also by five of the eight patients operated on (63%) having the lesion in the fourth ventricle where surgical removal is known to entail higher risks. The management of these patients requires meticulous diagnostic work-up and evaluation of morbidity during the natural course of the disease weighted against the risks of surgical removal. The development of laboratory tests or new imaging modalities allowing a lesion that is about to bleed to be recognized even in asymptomatic patients would be an invaluable aid in a neurosurgeon’s decision-making on how to manage a particular patient. Seven patients (21%) were admitted as emergencies with progressive worsening of symptoms, including epilepsy, headache, nausea, or focal neurological deficits (Table 19). Two patients had significant memory deficits, confirmed by neuropsychological testing. This patient was considered a statistical outlier and omitted from further analyses. The largest lesion (50mm) was a frontal cavernoma of type I that radiologically presented as a rare cystic form. In two patients, the measurement and radiological classification of the lesions were unreliable. One had a conglomerate of cavernomas on the parietal region with growth even through the parietal bone, and the other had numerous skin and bone cavernomas in the craniofacial region and in other organs (blue rubber bleb nevus syndrome). Three had numerous small lesions of 84 different radiological types, making removal practically impossible. In six patients, the risks of microsurgical removal were considered too high because of eloquent location. Surgical treatment was carried out in patients with hemorrhagic and/or epileptogenic cavernomas that had led to neurological deficits or drug-resistant epilepsy and that could be safely removed. In the majority of cases, the removed cavernoma was the largest lesion and usually with signs of recent bleeding. One of them had three consecutive bleedings from both lesions, which were located in the medulla oblongata close to each other and removable with the same approach. Another patient suffered from temporal complex partial seizures, with transformation to generalized seizures, and the frontal and temporal lesions on the right side were removed via a frontotemporal approach. Gross total removal of the symptomatic lesion was accomplished in 26 of 30 cases (86. In three patients, a lesion could not be localized and removed despite use of neuronavigation, and these patients refused further procedures. One patient underwent partial resection of the lesion, which however, remained stable during follow-up. One patient had numerous lesions in the parietal convexity, with extra and intracranial growth through the parietal bone and along the left side of the falx suggesting meningiomas, but surprisingly histology revealed a cavernoma. No statistically significant difference in Glasgow Outcome Score was observed between nonsurgical and surgical patients at follow-up (Pearson’s chi-square test, p>0. Postoperatively, one patient experienced temporary hemiparesis, and another patient developed mild expressive dysphasia that persisted over the four-year follow-up. All of them presented with acute severe headache that did not lead to any permanent neurological deficits or death. A patient with 532 cavernomas suffered from three symptomatic bleedings during nine years of follow-up. She recovered well from the hemorrhage-related focal neurological deficits but developed moderate disability due to progressive psychiatric disorders requiring long-term hospitalization. Fifteen patients suffering from seizures were operated on and three were treated conservatively. Of the three nonsurgical patients, one was seizure free at follow-up whereas two had occasional epileptic seizures despite anticonvulsant therapy. In patients with Engel I outcome, only minimal doses of anticonvulsants were recommended. A decision of whether to operate or not and which lesion to remove may be difficult due to the rare possibility to excise all 86 lesions in the same session. Furthermore, lesionectomy of the “wrong” cavernoma would not alleviate symptoms, but may carry additional surgical risks. Although in our series, the biggest cavernomas were usually the most active and showed signs of recent bleeding, the remaining lesions may also bleed or cause epileptic disorder in the future. However, they possess some potential for transforming to more aggressive types [53]. Still, we cannot predict which lesion carries the risk for clinical manifestations and whether prophylactic removal of radiologically inactive cavernomas is advocated. No definitive recommendations exist on how frequently patients should be imaged for a timely diagnosis. The dynamic nature of cavernomas could be seen in up to 77% of patients, with lesions undergoing some volumetric changes [55]. If patients have symptoms supported also by radiological progress, aggressive treatment of the most active lesion may be warranted, especially in younger individuals. However, in 89% of our cases these lesions were de novo cavernomas and reflected radiological progression; similar data have been obtained by other authors [168, 169, 343]. Although we did not find a statistically significant difference in Glasgow Outcome Score between operated and nonoperated patients, we believe that surgical removal of the most aggressive “correct” lesion will diminish the overall hemorrhage and epilepsy risk, and thus, is beneficial for the patient. Epileptic seizures occurred in 41% of our patients, indicating surgery especially when epilepsy was drug-resistant. In 35% of the patients with seizures, the lesion had bled on admission, which was also an indication for surgery. Of the surgically treated patients, 67% were seizure-free at the last follow-up (Engel class I), and only minimal doses of antiepileptic drugs were 87 prophylactically used. Postoperative seizure-free state has also been reported to be associated with the number of preoperative seizures and female gender [57]. However, we found no significant correlations between outcome and gender or age of surgical patients, probably because of the relatively low number of patients in our study. Minimal invasiveness and a simple and rational approach to avoid any additional damage to the vasculature or parenchyma will ensure uneventful postoperative course. Spinal cavernomas Patients and symptoms Basic characteristics of the patients are presented in Table 12. In nine patients (63%), the cavernomas were intramedullary, while four patients (29%) had an extradural lesion (Table 20) and one patient [156] had an intradural extramedullary cavernoma with an isolated intramedullary hemorrhage (Figure 22). The median age at presentation was 45 years (range 20 57 yrs), with an equal number of women and men. The median duration of symptoms before admission to our department was one year (range 24 hrs -14 yrs). Table 20 Presentation of intra and extramedullary cavernomas Characteristics Intramedullary Extramedullary (%) (%) Number of patients 9 (63) 5 (37) Symptom progression fast 4 (45) 4 (80) slow 5 (55) 1 (20) Hemorrhage yes 6 (67) 1 (20) no 3 (33) 4 (80) Patients suffered from sensorimotor paresis, radicular pain, or neurogenic micturition disorders in different combinations or separately as follows, a) Cervical region cavernomas (six patients): two suffered from severe tetraparesis, two presented with Brown-Sequard syndrome with ipsilateral paresis and contralateral pain and temperature loss below the lesion, and two had upper extremity 88 Figure 22 Case of extramedullary intradural cavernoma (arrow) causing intramedullary hemorrhage sensorimotor deficits accompanied by severe radicular pain. Bladder functions were impaired significantly in only one patient, b) Thoracolumbar region cavernomas (seven thoracic and one conus medullaris lesion): four patients presented with paraparesis combined with bladder dysfunction and numbness. Others suffered from drug-resistant radicular pain, numbness, and motor paresis of one of the lower extremities. Three patients (21%) presented with acute onset of symptoms, with rapid neurological decline indicating emergency surgical treatment. Five patients (36%) had a gradual progression of neurological deficits over one month preceding surgery and six patients (46%) had slow progression over more than a year. In two patients (14%), the symptoms improved before admission to our hospital, but surgery was performed to prevent hemorrhage and potential neurological decline. Four of them experienced acute neurological deterioration, warranting further investigations immediately after onset. However, two patients with hemorrhage did not have acute onset of the disease, deteriorating slowly over the course of several weeks.
Generic glucophage sr 500mg line
Most patients were primarily examined at the neurological department of the referring hospitals and thereafter sent to our neurosurgical center for further evaluation and treatment medicine cabinets surface mount cheap glucophage sr online master card. The collection of the series began in 2006, and the patient database was continuously supplemented by new cavernoma patients recruited to the study. Results of their treatment were assessed at a median of two, eight, three, and six years, respectively. The study protocol was approved by joint Ethical Committee of Helsinki University. Results Inraventricular cavernomas (n=12) the median age of our patients on admission was 47 years (range 15 – 66 yrs). As a presenting symptom, 11 patients (92%) had an acute mild to severe headache accompanied by nausea and vomiting. Four patients (36%) had hydrocephalus on admission, but shunting was necessary in only one patient. Patients with fourth ventricle cavernomas had a worse outcome than those with lateral-ventricle lesions. The largest lesion (50mm) was a Zabramski type I frontal cavernoma that had radiologically presented as a rare cystic form. In the majority of cases, the removed cavernoma was the largest lesion, and usually with signs of recent bleeding. Spinal cavernomas (n=14) the median age at presentation was 45 years (range 20-57 yrs). In nine patients (63%), the cavernomas were intramedullary, while four patients (29%) had an extradural lesion and one had an intradural extramedullary cavernoma with an isolated intramedullary hemorrhage. Patients suffered from sensorimotor paresis, radicular pain, or neurogenic micturition disorders in different combinations or separately. Three patients (21%) presented with acute onset of symptoms and rapid neurological decline necessitating emergency surgical treatment. Indications for microsurgical removal of a spinal cavernoma were progressive neurological deterioration in 12 patients (86%) and prevention of bleeding and consequent neurological decline in the remaining two patients (14%). At discharge, ten patients (71%) experienced improvement of their neurological status, three patients (21%) had worsening of the symptoms or some new deficits, and one patient remained the same. An extramedullary location proved to be better and safer regarding outcome: four of these five patients (80%) demonstrated further improvement of the symptoms, whereas only four of eight (50%) with an intramedullary lesion did the same. Temporal lobe cavernomas (n=53) the median age of patients at radiological diagnosis was 37 years (range 7-64 yrs). All ten patients with only one seizure preoperatively, were seizure-free at follow-up. Neither type, duration of seizures, nor location of the cavernoma inside the temporal lobe correlated with postoperative seizure outcome. Memory disorder was present in five patients with a history of epilepsy, but four of these patients already had this problem preoperatively. None of the asymptomatic patients developed neurological deficits postoperatively. Conclusions Microsurgical treatment of brain and spine cavernomas is safe and effective. Most operated patients with intraventricular, multiple, spinal, and temporal lobe cavernomas had significant improvement of their symptoms. Due to rareness of these lesions, a decision to operate may be difficult requiring vast experience and dexterity of the neurosurgeon. In patients with cavernomas of the fourth ventricle, surgical risks are higher than with cavernomas of other ventricles. In cases of multiple cavernomas, removal of epileptogenic cavernomas is beneficial but antiepileptic drugs are used due to the remaining lesions. Spinal intramedullary cavernomas carry higher risks of permanent neurological deficits than those in extramedullary location. In these patients, the worst prognosis was linked to bladder disorders, which occurred in 43% of patients despite surgical treatment. In cases of temporal lobe cavernoma, favorable seizure-outcome after lesionectomy is expected. Kivelev J, Niemelä M, Kivisaari R, Hernesniemi J: Intraventricular cerebral cavernomas: a series of 12 patients and review of the literature. Kivelev J, Niemelä M, Kivisaari R, Dashti R, Laakso A, Hernesniemi J: Long-term outcome of patients with multiple cerebral cavernous malformations. Kivelev J, Niemelä M, Hernesniemi J: Outcome after microsurgery in 14 patients with spinal cavernomas and literature review. Kivelev J, Niemelä M, Blomstedt G, Roivainen R, Lehecka M, Hernesniemi J: Microsurgical treatment of temporal lobe cavernomas. They are usually detected between the second and fifth decade of life [57, 256, 343]. The latter are more frequent in Hispanic-Americans, accounting for up to 50% of cavernomas [254]. In contrast, among Caucasians, the familial forms are encountered in only 10-20% of patients [254, 259]. Patients with familial forms are typically affected by multiple cavernomas, whereas sporadic forms mostly present with a single lesion. In hereditary cases, cavernomas are characterized by an autosomal-dominant pattern of inheritance with incomplete penetrance. Three genes responsible for development of the cavernomas have been identified to date [60, 80, 130, 170]. When their mutations express, loss of respective proteins leads to formation of the lesion, with dilated thin-walled sinusoids or caverns covered by a single layer of endothelium that has undeveloped interstitial junctions and subendothelial interstitium [193, 334]. Blood flow inside the sinusoids is low, predisposing to intraluminal stasis and thrombosis. Due to fragility of the sinusoid wall, a cavernoma causes repetitive microhemorrhages into the surrounding neural tissue with formation of perifocal hemosiderosis and reactive gliosis. Such local homeostatic instability produced by either genetic or reactive environmental factors (inflammation, breakdown of the blood-brain barrier, gliosis) may provoke intensive neoangiogenesis and proliferation of the sinusoids. Subsequently, lesions enlarge and grow, which may coexist with clinical progression. The natural history of brain cavernomas is relatively benign and up to 21% of patients are asymptomatic [132]. The most frequent manifestations of the disease are seizures, focal neurological deficits and hemorrhage. Seizure activity occurs in up to 80% of patients with supratentorial cavernomas most probably being evoked by perilesional intraparenchymal changes [15, 71, 223, 256, 288]. Focal neurological deficits are typical for cavernomas located close to eloquent regions of the brain and for spinal lesions. Headaches are fairly common complaint in many cavernoma patients, and usually lead to further clinical and radiological work-up. However, due to their unspecific nature, headaches are not linked to the cavernoma in every patient and frequently represent some other clinical condition. An acute exacerbation of the symptoms of any clinical pattern of cavernomas is prevalently related to hemorrhage. In most patients, bleeding is not life-threatening, but, in certain cases, it can cause devastating neurological deficits. Furthermore, the risk of re-bleeding increases from 5% to 60% per patient 14 year [90, 94, 235, 327] indicating active treatment of the lesion in early stages after the first event. Microsurgical removal of the symptomatic cavernoma is generally accepted as the most effective and safe method. Most operated patients with a lesion in a safely accessible location usually gain convincing relief of their symptoms. Nevertheless, deep or eloquent sites of the brain and intramedullary spine location increase surgical invasiveness and risks of postoperative complications. In the present work, data on all consecutive patients suffering from cavernoma and treated at the neurosurgical department of Helsinki University Central Hospital during the last 30 years have been analyzed. Due to the limited literature on intraventricular, spinal, multiple, and temporal lobe cavernomas, these entities were reviewed more extensively. Luschka classified angiomas into two types: 1) those arising by sequestration of a small portion of the embryonic capillary vascular system; and 2) “true tumor” formation originating from vascular tissue. His own case belonged to the latter type and was a cavernoma according to the modern definition of this term.
Syndromes
- Is your body blue all over?
- Using a special lens to look at the eye (gonioscopy)
- Breathing difficulty (from breathing in dye remover)
- Severe dry eye associated with arthritis (keratoconjunctivitis sicca)
- Appetite decrease and weight loss
- Chemotherapy drugs
- Near Optimal: 100 - 129 mg/dL
Generic glucophage sr 500 mg on line
A treatment that utilizes an intravascular approach would eliminate the concerns regarding drug delivery through the blood-brain or blood tumor barrier medicine 751 purchase glucophage sr visa. Extensive investigations of bevacizumab clearly demonstrate anticancer activity in a variety of systemic cancers, including renal cell carcinoma, non-small cell lung cancer, and colorectal cancer (Yang, Haworth et al. In most studies, bevacizumab was used in combination with traditional cytotoxic agents. Randomized trials suggest that there is benefit in combining bevacizumab with cytotoxic chemotherapy drugs compared with the cytotoxic regimen alone (Gille 2006). Although the mechanism of treatment enhancement is unknown, two main hypotheses have been proposed. The second hypothesis proposes that bevacizumab selectively inhibits angiogenesis and results in the loss of markedly aberrant and tortuous intratumoral neovasculature, causing a paradoxical improvement in perfusion and delivery of the cytotoxic agent to the tumor cells. Available data support both theories, and both mechanisms may be responsible for the proven benefit of bevacizumab in the wide spectrum of cancers tested to date. There have been small series and anecdotal reports of patients with recurrent malignant glioma, predominantly glioblastoma, who have been treated with the combination of irinotecan and bevacizumab (Stark-Vance 2005; Vredenburgh, Desjardins et al. A high objective response rate has been noted, and in some cases the responses appear to be durable. The investigators reported a 57% objective response rate and a 6-month progression-free survival rate of 46%. The results of both studies compare very favorably with single-agent temozolomide in patients with no prior temozolomide exposure, where objective tumor responses were reported in less than 6% of patients and the 6-month progression-free survival rate was 21% (Yung, Albright et al. Despite concerns regarding the potential for intratumoral hemorrhages, particularly in light of an early report of bleeding in a brain metastasis in a patient on a clinical trial with bevacizumab, the preliminary reports suggest that this complication is infrequent in gliomas. Similarly, the large trials of bevacizumab in colorectal, lung, and breast cancer suggest an increase in vascular thrombotic events, although the excess numbers appear to be arterial thromboses. Again, this problem has not been identified in the brain tumor population treated with bevacizumab. Overall response rate, as determined by independent radiology review, was 20% in the bevacizumab alone arm and 33% with the combination. The 6-month progression-free survival rate was 35% for bevacizumab alone and 50% for the combination. Although the study was not statistically powered to compare the two arms, these results suggest a response and progression-free rate benefit to the combination of bevacizumab with a cytotoxic agent. Laboratory and clinical imaging studies also support the potential role of antiangiogenic agents in combination with both radiation therapy and chemotherapy (Batchelor, Sorensen et al. Contrary to the early concerns that these agents would markedly reduce blood flow and therefore delivery of oxygen (for radiation-induced free radical formation) and delivery of chemotherapy, studies now clearly demonstrate that antiangiogenic agents cause vascular normalization (Jain 2005). Tumors typically demonstrate extensive neovascularization that is characterized by tortuous vessels, poorly formed basement membranes, and often by saccular structures (dead ends) and large gaps between endothelial cells. Antiangiogenic agents have been shown to eliminate many of these poorly formed vascular components, resulting in an overall enhancement of blood supply to the tumor through a process called “vascular normalization. Preliminary results from a neoadjuvant trial in patients with rectal cancer demonstrated a decrease in blood perfusion/permeability and interstitial fluid pressure in tumors after one dose of bevacizumab (Willett, Boucher et al. Fertility may be impaired in cynomolgus monkeys administered bevacizumab, which led to reduced uterine weight and endometrial proliferation as well as a decrease in ovarian weight and number of corpora lutea. In juvenile cynomolgus monkeys with open growth plates, bevacizumab induced physeal dysplasia that was partially reversible upon cessation of therapy. Bevacizumab also delays the rate of wound healing in rabbits, and this effect appeared to be dose dependent and characterized by a reduction of wound tensile strength. The estimated half-life of bevacizumab is approximately 21 days (range 11-50 days). The maximum tolerated dose of bevacizumab has not been determined; however, the dose level of 20 mg/kg was associated with severe headaches (Cobleigh, Langmuir et al. The study demonstrated a highly significant prolongation of time to progression in the high-dose arm (4. The tumor response rate was 10% in the high-dose arm but was 0% in the low dose and placebo groups. Additional clinical trials are ongoing in a variety of solid tumors and hematologic malignancies using bevacizumab as monotherapy or in combination with chemotherapy, radiation, or other targeted/biologic agents. Clinical trials have been reported using bevacizumab in combination with irinotecan to treat patients with recurrent malignant glioma. Stark-Vance reported the first study in 2004 at the World Federation of Neuro-Oncology. Twenty-one patients were treated and an objective response rate, as determined by changes in cross-sectional area was demonstrated (Stark-Vance 2005). Treatment was reportedly well tolerated, although six patients were removed from the study because of medical issues, two of which were believed related to treatment (thrombosis and intestinal perforation). The investigators reported a 57% objective response rate and a 6-month progression free survival rate of 46%. They report one intracranial hemorrhage among 35 treated patients and 4 incidents of thromboembolic complications. Initial studies evaluated the efficacy of temozolomide in patients with recurrent glioblastoma and anaplastic glioma. The study demonstrated only a modest objective response rate for both regimens (approximately 5%), but a superior 6-month progression-free survival rate for temozolomide (21% vs. However, the responses were not durable in many cases and the median progression-free survival rate was 3. This suggests that the neoadjuvant temozolomide chemotherapy likely had little overall benefit. However, these results did demonstrate definite activity of temozolomide for glioblastoma (Gilbert, Friedman et al. There were no published studies using temozolomide as a post-radiation adjuvant treatment. Treatment was well tolerated and the study demonstrated a statistically significant improvement in median survival, progression free survival, and 2-year survival rate for the combination treatment (Hegi, Diserens et al. Recently there has been some concern that health-related quality of life assessments may reflect patient ‘response shift,’ as they frequently measure patient preferences and adjustment in terms of their function. It has demonstrated reliability and validity in the primary brain tumor patient population, including predictive validity for tumor recurrence. Assessment of neurocognitive function provides unique information about neurologic function that frequently is not captured by self-report measures (Cull 1996). Brain tumors affect brain functioning, and interventions such as chemotherapy and radiation therapy may also impact on brain functions. Therefore, tumor recurrence, survival, and time to progression end points in a clinical trial may not fully describe the outcome of an intervention unless added information regarding neurocognitive function, health-related quality of life, and symptom assessments are also considered as therapeutic outcomes. The arguments for including neurobehavioral measures as an index for determining treatment outcomes for brain tumor patients have been recently reviewed (Weitzner 1997). Neurocognitive function has been demonstrated to predict tumor progression (Meyers 2003) and to independently predict survival for patients with central nervous system tumors (Meyers 2000, Meyers 2004, Taphoorn 2004). A brief, sensitive, repeatable, highly standardized battery of cognitive tests has been utilized in numerous brain tumor clinical trials (Groves 1999, Levin 2002). This battery has also been demonstrated to be practical in terms of cost and burden to the patient, with good compliance in multicenter trials (Meyers 2004). An important endpoint in this study is to evaluate the neurocognitive, symptom and quality of life profile across the disease course. This includes assessments during the early phase when the majority of patients may demonstrate a differential treatment effect of one treatment approach relative to the other and during the late period when the subgroup of long term survivors may experience impact on their neurocognitive function, symptoms and quality of life. Encephalopathy has been reported as an acute adverse side effect in glioma patients treated with bevacizumab and radiation. In addition, leukoencephalopathy has been reported in patients with systemic cancer treated with this agent. This study will provide an opportunity to collect this important data and have a control group that was not treated with this agent. By marrying these assessments with imaging, we will be able to study the correspondence between imaging and non-imaging biomarkers and distinguish changes that are treatment related from those associated with recurrent tumor. An additional issue with this treatment is the reported change in the pattern of recurrence, from a localized mass to a more infiltrative pattern. The potential neurocognitive and neurologic symptom impact of this change has not yet been defined. Collecting this information on long-term survivors on this trial will provide an opportunity to document any impact on neurocognitive function, symptoms, and quality of life.
Buy genuine glucophage sr online
Women whose birth control contains hormones should speak with their doctors about switching to a form of birth control that is hormone-free symptoms for mono 500mg glucophage sr. Hair loss (alopecia): Although not all chemotherapy drugs cause hair loss (alopecia), many of these drugs induce significant hair loss or baldness. As a result of the cooling system, blood vessels in the scalp constrict, resulting in decreased hair follicle activity which helps reduce hair loss. Typically, when one type of chemo fails, their doctor puts them on another chemo drug, then another, ad infinitum. Since chemo drugs can cause considerable side effects, their cumulative effect upon the patient needs to be carefully considered. Although there is no hard and fast rule regarding when to stop chemotherapy (and possibly [re-] try a different type of therapy such as hormonal, targeted, or immunotherapy, or cease treatment altogether), the author located the following studies: A retrospective review of randomized studies compared shorter versus longer chemotherapy. These studies have generally shown that prolonged treatment is associated with extended Time to Progression but has little effect on Overall Survival. A recent systematic review of eight randomized trials including 1,942 patients demonstrated no significant reduction in the risk of death with prolonged therapy. When chemotherapy is given for these reasons, it is called palliative chemotherapy. Not much research has looked at whether palliative chemotherapy for end-stage disease actually succeeds in improving quality of life. At the beginning of the study, the researchers asked the people in the study about their quality of life as well as their level of well-being, both physically and psychologically. The researchers also asked the caregiver most familiar with the person’s well-being to do the same assessment. After a person died, the researchers asked the caregiver to rate the person’s quality of life in the last week of life. The caregivers’ assessments were considered accurate because their assessments matched the people’s self-assessments when the study started. For patients who were the sickest and had a lower quality of life when the study started, the caregiver rating of their last week of life was about the same, whether or not the people had received palliative chemotherapy. So, the end-of-life chemotherapy didn’t seem to improve quality of life for these people. And for people who were in relatively good health and had better quality of life when the study started, more than half (56%) had worse quality of life in their final week of life after receiving palliative chemotherapy. There was no difference in survival between the people who received palliative chemotherapy and those who didn’t. In general, guidelines generally indicate that chemotherapy should be stopped if there were no benefits from three back-to-back regimens, and/or when it is determined or felt that these regimens are doing more harm than good. That said, treatment decisions for end-stage cancer are extremely personal and individualized and need to be discussed in detail with one’s medical team. It’s important for patients to speak with their doctors, family, and other loved ones. Some people prefer to receive treatment up until the last day of their lives, while others will stop and prefer to spend the last weeks or months of their lives with their families, with their pain and other symptoms controlled without chemotherapy. Microtubule Inhibitors such as Docetaxel, Eribulin, Ixempra, Paclitaxel and Navelbine stop cells from dividing into two cells. Treatment should be based on previous therapy, differential toxicity, other medical conditions, and patient preferences. In a minor surgical procedure, the port is implanted, which means it is placed completely beneath the skin, and the catheter is inserted inside a blood vessel. The port allows the doctor or nurse to deliver medications and fluids or withdraw blood samples without having to stick the patient’s vein with a needle. People who tend to form blood clots, have a body size that will not allow for proper port placement or access, or have had radiation to the site where the port is intended to be placed may reconsider having a port. Tunneled Catheters: this type of catheter is surgically inserted into a vein in the neck or chest and passed under the skin. This is because the patient may receive significant benefits with fewer side effects with just one drug. Below is information about pre-testing tumor cells prior to administering taxane treatment, along with a comparison of the three taxane drugs. Therefore, patients considering a taxane-based regimen may wish to discuss the following research with their doctor. Researchers at Sanford-Burnham Medical Research Institute have discovered a mechanism that explains why some breast cancer tumors respond to specific chemotherapies and others do not. The findings highlight the level of glutamine, an essential nutrient for cancer development, as a determinant of breast cancer response to select anticancer therapies such as taxanes. Although researchers have been aware that many tumor cell types are dependent on glutamine for growth and survival, they did not know how glutamine uptake was regulated. We found that this interaction causes degradation of the glutamine carrier proteins, leading to an insufficient supply of glutamine and the sensitization of breast cancer tumors to death. Significantly, the Sanford-Burnham Medical Research Institute has begun screening for inhibitors of glutamine carrier proteins as a potential new target for breast cancer treatment. Taxol (Paclitaxel): Taxotere produced a 32% anti-cancer response compared with Taxol’s 25% response, and patients taking Taxotere had a 5. However, there is a small risk of permanent hair loss resulting from the use of Taxotere. Taxol (Paclitaxel): Abraxane produced a 33% anti-cancer response compared with Taxol’s 19% response (the 19% response rate to Taxol differed in this study from the 25% response rate in the above study). Only 9% of patients on Abraxane experienced neutropenia (an abnormally low count of neutrophils which area type of white blood cell that helps fight off infections), whereas 22% of patients taking Taxol had neutropenia. Whereas Taxol is administered with a toxic chemical solvent (liquid solution) in addition to the drug, Abraxane uses nanoparticle albumin-bound (“nab”) technology. This technique uses albumin, the most abundant protein in the body, to deliver the drug directly to cancer cells. With Abraxane, 50% more of the drug can be administered, more of the active drug is transported into the cancer cells, and patients generally experience fewer side effects. Taxane drugs include Taxol (Paclitaxel), Taxotere (Docetaxel), and Abraxane (Nab-Paclitaxel; Protein-Bound Paclitaxel). Therefore, patients who have taken, or are taking, a Taxane drug should be especially vigilant about reporting symptoms such as headaches, blurred vision, speech or cognitive difficulties, numbness, and/or dizziness to their physician. Xeloda may cause “Hand Foot Syndrome,” which is evidenced by peeling and/or blistering of skin on the hands and feet. Data presented in a retrospective review demonstrate that the dose of Xeloda can be reduced, either when used alone or in combination with docetaxel, to minimize adverse events without compromising efficacy in terms of Time to Progression or Overall Survival. In one study, 32 patients who had at least 2 prior chemo regimens received a median of 6 cycles of the drug. Patients should ensure that their doctors order tests before and during treatment to check whether their heart is working well enough to safely receive these drugs. The use of a specific agent can be repeated if recurrence happens more than 12 months after the last treatment. This conversation should also include specific examples as to when patients should notify their doctor immediately or go to the Emergency Room (such as if the patient is experiencing difficulty breathing). Patients are also encouraged to visit the drug’s website to learn more about the drug(s) and potential side effects, and to ask their doctor about other therapies if they are concerned about taking a particular drug(s). And as always, before taking any new drug, patients must make sure to tell their doctor about their medical history, other medications and supplements they are taking, and any concerns they may have. At this point, other options such as chemotherapy (and potentially clinical trials) should be considered. In some cases, a listed drug can be combined with another drug as described in the Hormone Receptor Positive Breast Cancer section of this Guide. But because they are “selective,” they allow estrogen to communicate with other cells (such as bone, liver and uterine cells) that also have estrogen receptors. Fulvestrant may be given alone or paired with Ibrance, Kisqali, or Verzenio in specific circumstances. The “estrogen paradox” refers to the fact that on the one hand estrogens are known to stimulate the growth of breast cancer, whereas on the other hand high doses of estrogens are an effective treatment for this disease. When estrogen-lowering drugs no longer control metastatic breast cancer, the opposite strategy might work. Clinical benefit was observed in 5 patients (26%), and all five of these patients had stable disease ≥6 months. Not only did estrogen treatment often stop disease progression, in some patients’ metastatic tumors became “re-sensitized” and again responded to anti-estrogen treatment.
Cheap glucophage sr 500 mg mastercard
Semantic impairment symptoms 7 days after conception discount glucophage sr 500mg fast delivery, hypoperfusion of the temporal cortex, bilateral but with a left predominance. The Parkinsonian features are related to movement disorders such as rigidity, reduced speed and uncontrolled movemements, including those of the eye (supranuclear palsy). Symptoms and course Clinical presentation is extremely variable, according to the type of mutation on tau gene, and heterogeneous inside a same family. Patients may have slowly progressive behavioural changes, language disturbances, and/or extrapyramidal signs. Some have with rigidity, bradykinesia, supranuclear palsy and saccadic eye movement disorders. Symptoms usually start between 40 and 60 years of age, but may occur earlier or later. Disease duration is usually between five and ten years, but occasionally may be up to 20-30 years. Genetics Familial autosomic dominant, with full penetrance (One child out of two inherits of the mutation of the parent, and this mutation will inevitably provoke the disease). Care and treatment As yet there is no cure for fronto-temporal dementia and the progression of the condition cannot be slowed. Ongoing research / clinical trials these mutations have generated the concept of “tauopathies”, since the cause of the disease is tau mutations. PiD is characterised by specific lesions named Pick bodies that are found in the hippocampus and in the neocortex. This could be linked to difficulty in identifying emotions shown by their relatives. Although the disease varies greatly in the way it affects individuals, there is a common core of symptoms among patients, which may be present at different stages of the disease. These symptoms include loss of memory, lack of spontaneity, difficulty in thinking or concentrating, and disturbances of speech. Other symptoms include gradual emotional dullness, loss of moral judgment, and progressive dementia. Causes and risk factors A specific neurofibrillary degeneration, revealed by the presence of Pick bodies in the hippocampus and fronto-temporal cortex and an abnormal processing of tau proteins, is associated to this pathology. Diagnostic procedures Clinical with the specific features of fronto-temporal impairment. Ongoing research / clinical trials Like most fronto-temporal dementia, tau proteins seem to be involved in the aetiology of the disease. However, levels of normal tau protein are dramatically decreased, suggesting that this fronto-temporal dementia is also a tauopathy (“tau-less tauopathy”: Zhukareva et al, 2001). Typically, during the initial stages of fronto temporal dementia, memory will still be intact, but the personality and behaviour of the person will change. The person may lose their inhibitions and become extrovert, or alternatively may become apathetic and withdrawn. They may become aggressive which may be quite out of character, and may develop fixed routines. However sometimes difficulties in organisation and concentration may lead to an apparent memory problem. Those affected may no longer recognise friends and family and may need nursing care, become incontinent and bed-ridden. Ongoing research / clinical trials Research on the physiopathology of tau proteins, likely involved in the process Available services the Association for Frontotemporal Dementias. Other common symptoms include rigidity and backward arching of the neck, and a key diagnostic feature the "Supranuclear Palsy". Tiny, cramped handwriting and some changes in personality are often other indicators of the disease. Cognitive symptoms include reduced verbal fluency, attention deficit, executive dysfunction, slowing of information processing and problems with complex and abstract thought. From a broad survey of various countries in the Western World, the probability of the disease being passed from one generation to the next within a family is extremely low. However, as observed in many neurodegenerative disorders, tau proteins or tau gene is likely a significant causal factor. Levodopa and anticholinergic medications may provide temporary reduction of symptoms. A randomised, multicentric, double blind, placebo controlled, stratified, parallel group study. The cortex, or outer layer of the brain, is severely affected, especially the fronto-parietal regions, located near the center-top of the head. Other, deeper brain regions are also affected, including parts of the basal ganglia, hence the name "corticobasal" degeneration. Symptoms include signs of parkinsonism such as poor coordination, akinesia (an absence of movements), rigidity (a resistance to imposed movement), and disequilibrium (impaired balance); and limb dystonia (abnormal muscle postures). Other symptoms such as cognitive and visual-spatial impairments, apraxia (loss of the ability to make familiar, purposeful movements), hesitant and halting speech, myoclonus, and dysphagia (difficulty swallowing) may also occur. A degeneration affecting many subcortical nuclei and spreading into the neocortex in the frontal and parietal areas with an aggregation of tau protein in affected areas within neurons and in astrocytes. Belongs to the 4R tauopathies (aggregation of tau isoforms with 4 repeats) (Sergeant N. Care and treatment Unfortunately, there are no drugs or other therapies that can slow the progress of the disease, and very few that offer symptomatic relief. A sporadic late-onset form of dementia characterised by a neuro-degenerative process, which mainly affects limbic structures (amygdala, hippocampus and mediobasal temporal/entorhinal cortex). It is named after silver-staining (argyrophilic) grains or "coiled bodies" within the cytoplasm of neurons that consist mainly of tau protein isoforms with four microtubule-binding repeates (4-R tau). Causes and risk factors Neuron degeneration likely associated with dysfunction of tau protein. Diagnostic procedures It is almost impossible to distinguish from late-onset Alzheimer’s disease. Available services Due to the recent characterization of this disease, there are no specific available services. Argyrophilic grain disease: neuropathology, frequency in a dementia brain bank and lack of relationship with apolipoprotein E. Argyrophilic grain disease: widespread hyperphosphorylation of tau protein in limbic neurons. The disorder is characterized by postural (or orthostatic) hypotension—an excessive drop in blood pressure when the patient stands up, which causes dizziness or momentary blackouts. Orthostatic hypotension and symptoms of autonomic failure such as constipation, impotence in men, and urinary incontinence usually predominate early in the course of the disease. For the majority of patients, blood pressure is low when the patients stand up and high when the patients lie down. Other symptoms that may develop include impaired speech, difficulties with breathing and swallowing, and inability to sweat. Shy-Drager syndrome usually ends in the patient’s death by 7 to 10 years after diagnosis. Breathing problems such as aspiration, stridor (high-pitched breathing sounds due to airway obstruction), or cardiopulmonary arrest are common causes of death. Causes and risk factors Neurodegeneration in subcortical nuclei is mainly affecting oligodendrocytes. Frequency the average annual incidence rate (new cases per 100,000 person-years) for ages 50 to 99 years is 3. Diagnostic procedures the diagnosis is mainly based on the specific clinical manifestations (postural or orthostatic) hypotension, rigidity, balance, coordination, impaired speech, excessive drop in blood pressure, and in general autonomic/urogenital failure. To relieve low blood pressure while standing, dietary increases of salt and fluid may be beneficial. Medications to elevate blood pressure, such as salt-retaining steroids, are often necessary, but they can cause side effects and should be carefully monitored by a physician. Alpha-adrenergic medications, non-steroidal anti-inflammatory drugs, and sympathomimetic amines are sometimes used.
Glucophage sr 500 mg overnight delivery
A tl as f u an at y N vartis J ack s symptoms synonym purchase cheapest glucophage sr and glucophage sr, S i r ss S ecti al I m agi g M ade E asy hurchi l l L ivi gst e, 2. Clinical evidence is reviewed as it pertains to stroke lesion location (cerebral, right & left hemispheres; lacunar and brain stem), related disorders (emotional, visual spatial perceptual, communication, fatigue, etc. Robert Teasell Parkwood Institute, 550 Wellington Road, London, Ontario, Canada, N6C 0A7 Phone: 519. The impairments associated with a stroke exhibit a wide diversity of clinical signs and symptoms. Disability, which is multifactorial in its determination, varies according to the degree of neurological recovery, the site of the lesion, the patient’s premorbid status and the environmental support systems. Certain types of strokes tend to occur in specific areas; for instance, lacunar infarcts occur most often in subcortical regions (Dombovy, 1991). The most common presentation of a stroke patient requiring rehabilitation is contralateral hemiparesis or hemiplegia. Other neurological manifestations will vary depending upon the side of the stroke lesion and whether the stroke occurs in the cerebral hemispheres or the brainstem (See Figure 2. This explains greater arm involvement in a middle cerebral artery occlusion and greater leg involvement in an anterior cerebral artery occlusion. There is a large degree of specialization within the brain with different neurologic functions divided amongst the two hemispheres and the brainstem. The clinical picture of a stroke depends upon which specialized centers have been damaged with subsequent loss of the specialized neurological function they control. Even a simple activity, such as bending over to pick up an object, requires the integrated function of the entire central nervous system. When damage occurs in one region of the brain, not only are those specialized centers associated with the impaired region affected, but also the entire brain suffers from loss of input from the injured part. The arterial territory affected will determine the clinical manifestations; hence, localization of a stroke is often described in such terms. This is best understood by dividing the brain into the cerebral hemispheres, where all but the posterior hemispheres are supplied by the (carotid/anterior circulation), left and right side, and the brain stem and posterior hemispheres (vertebral basilar/posterior circulation) (Figure 2. Middle cerebral artery involvement is very common while anterior cerebral artery strokes are less common (Teasell, 1998). The middle cerebral artery covers two-thirds of the lateral surface of the cerebral hemisphere (Kiernan, 1998; Scremin, 2004). This vascular territory includes the medial aspect of the frontal and parietal lobes, the anterior half of the internal capsule, the anterior inferior head of the caudate, and the anterior four fifths of the corpus callosum. The territory also includes the supplementary motor area and the primary motor and sensory areas for the contralateral lower extremity (see Figure 2. The Circle of Willis often compensates for lesions proximal to the anterior communicating arteries. Bilateral lesions Incontinence, abulia or slow mentation and the appearance of primitive reflexes. Proximal occlusion All of the above signs plus facial and proximal arm weakness and frontal apraxia, with left side involvement. Interruption of Commissural Sympathetic apraxia of the left arm, right motor paresis. In North America, the etiology of this infarction is generally embolic rather than atherothrombotic (Adams, 1997). However, an atherothrombotic infarction of the internal carotid artery invariably presents with 2. The clinical consequences are similar to those with involvement of the anterior/carotid circulation (see above). Additional clinical signs and symptoms occur depending on whether the right or left hemisphere is involved. Left Hemispheric Lesions Each hemisphere is responsible for initiating motor activity and receiving sensory information from the opposite side of the body. However, as mentioned previously, each hemisphere has a large degree of specialization. Despite this specialization, normal thinking and carrying out of activities requires the integrated function of both hemispheres, neither of which is truly dominant over the other. Many stroke patients have diffuse cerebrovascular disease and other conditions resulting in impaired cerebral circulation. While there may be one major area of infarction, there may be other areas of ischemic damage located throughout the hemispheres that may complicate the clinical presentation. Clinical signs and symptoms include visual-spatial perceptual deficits, emotional disorders and subtle communication problems. Therefore, in a right hemisphere middle cerebral infarct, visual-spatial perceptual disorders include left-sided neglect, figure ground disorientation, constructional apraxia and asterognosis (the later seen with left hemisphere disorders). The most commonly seen visual-perceptual spatial problem is the unilateral neglect syndrome. Kwasnica (2002) noted that, “they often do not orient to people approaching them from the contralateral side (Rafal, 1994). Patient may be noted not to dress the contralateral side of the body, or shave the contralateral side of the face. Some may fail to eat food on the contralateral side of their plates, unaware of the food they have left (Mesulam, 1985). Chronically, it is rare to see significant unilateral neglect following stroke (Kwasnica, 2002). He found that neglect, as measured by failure to spontaneously attend to stimuli on the left, had a median time to recovery of nine weeks; approximately 90% of the patients recovered by 20 weeks. He also measured unilateral spatial neglect, scored from a drawing task; 70% of patients recovered in 15 weeks. In chronic stroke patients unilateral neglect is usually subtle and may only be seen when competing stimuli are present, such as a busy therapy gym where patients may find it difficult to direct their attention to a therapist on their left side” (Kwasnica, 2002). Defined as a failure to report, respond, or orient to sensory stimuli presented to the side contralateral to the stroke lesion. More obvious forms of neglect involve colliding with environment on involved side, ignoring food on one side of plate, and attending to only one side of body. More subtle forms are more common, more apparent during high levels of activity such as driving, work, or interacting with others. Milder neglect involves various degrees of ignoring the affected side when faced with stimulation on the unaffected side (extinction). These patients can fail to notice their contralesional limbs, whether or not they are hemiparetic. They also frequently deny their hemiplegia or minimize its impact on their functional status. This exists in as much as 36% of patients with right hemisphere strokes” (Hier et al. Recovery from constructional and dressing apraxia was intermediate while recovery was slowest for hemiparesis, hemianopsia and extinction. Such perceptual impairments have been shown to adversely influence the rate of achieving independent sitting and stair climbing (Mayo, Korner-Bitensky, & Becker, 1991). Difficulties generally labeled as emotionally related include indifference reaction or flat affect, impulsivity (often leading to multiple accidents) and emotional lability. Annett (1975) demonstrated aphasia occurred after right hemispheric strokes in 30% of left-handed people and 5% of right-handed people. Moreover, patients with nondominant hemispheric lesions often have associated communication difficulties, whereby they have difficulty in utilizing intact language skills effectively, that is, the pragmatics of conversation. The patient may not observe turn-taking rules of conversation, may have difficulty telling, or understanding, jokes (frequently missing the punchline), comprehending ironic comments and may be less likely to appropriately initiate conversation. This tends to result in social dysfunction that may negatively impact on family and social support systems (Delaney, 1993). Clinical signs and symptoms include aphasia, apraxia, and arguably emotional disorders. Therefore 97% of the population has language control primarily in the left hemisphere. Language function is almost exclusively the domain of the left hemisphere, except for 35% of left handers (3% of population) who use the right hemisphere for language function. Good Poor Yes No Yes No No Transcortical Mixed Conduction Transcortical Motor Broca’s Transcortical Global Sensory Wernicke’s Figure 2. Posterior-inferior frontal lobe stroke characterized by nonfluent, effortful speech with preserved comprehension and poor repetition.
Buy glucophage sr 500 mg with visa
All families are unprepared for brain injury and inexperienced in managing the many aspects of life after injury medicine pacifier order cheap glucophage sr line. Outcomes change over time: just as each of us changes, so do people with brain injuries. Many individuals adjust well to disability and go on to productive and satisfying lives. In general, given time and appropriate information most families accept what they cannot change. There will always be a minority of families, however, who will search endlessly for the special program, alternative treatment, or method to “fx” their family member. Families should never give up hope that science, technology and public awareness will ease the road ahead. Life goes on, albeit changed after brain injury, but the human spirit can move mountains. Become an Advocate An old German proverb says, “When one helps another, both are made strong. Networks of advocates have created programs and services of value to you and your family. At the larger level, legislative advocacy changes laws, and grassroots efforts affect every level of society. For example, although the term “traumatic brain injury” was frst mentioned in the Individuals with Disabilities Education Act of 1990, the frst formal act of Congress to acknowledge brain injury as a major disability population was not passed until 1996. That act—the Traumatic Brain Injury Act—was the direct result of brain injury advocates’ hard work. Once they are on the road to recovery, many people with brain injuries fnd great personal satisfaction in advocacy. Contributing time and talent to a cause offers great rewards for persons with brain injuries and their families and caregivers. Their efforts force change, however slowly, improving the lives of the over fve million Americans currently living with brain injury. Information and Resources the Web offers far more information on brain injury than could possibly be listed here. When you visit any of the following sites, check the links section for even more information. A free catalog can be requested online along with one free tip card for frst time customers. Links explore return to work, special programs benefting other members of the family and much more. The National Association of Head Injury Administrators Technical Assistance Center Although primarily for the use of grantees, it has interesting links under “who to contact. Some of the sites found there are sponsored by service providers, lawyers, and individuals wishing to share information through informational websites and chat rooms. She developed her expertise in brain injury following a 1982 auto crash in which her son sustained a severe traumatic brain injury. She is the author of Ketchup on the Baseboard, as well as numerous monographs and book chapters. She is the Founder of the Brain Injury Association of Florida and a member of the Traumatic Brain Injury Technical Assistance Center Steering Committee, U. Bruce Lifetime Achievement Award from the Florida Department of Health, Brain and Spinal Cord Injury Program. She is also the recipient of several major national awards: the 1994 Jim and Sarah Brady Award for Public Service; the Association of Trial Lawyers of America 1997 Civil Justice Foundation Community Champion Award; the 2004 John Young Lectureship, Craig Hospital, Englewood, Colorado, the 2005 David Strauss Memorial Lectureship, and the North American Brain Injury Society 2005 award for Public Policy and Advocacy. Its contents are solely the responsibility of the authors and do not necessarily represent that offcial views of the U. The treatment is directed towards not only metastatic brain tumors but their symptoms as well. Longer survival, improved quality of life and stabilization of neurocognitive function for patients with brain metastasis is the goal of treatment. There have been numerous advances in the treatment of metastatic brain tumors in the last decade. Lung, breast, melanoma (skin cancer), colon and kidney cancers commonly spread to the brain. Fewer than 10% of all brain metastases are found before the primary cancer is diagnosed. Occasionally, the person may have neurological symptoms, undergoes a brain scan and has no history of cancer when the brain tumor is detected. If the site of the primary cancer is not found, this is called an “unknown” primary site. Frequently, the primary site may have been too tiny to be seen or to cause symptoms. In that situation, the metastatic brain tumor is found and subsequently the primary site is discovered. Markers found in the blood, the appearance of the tumor on a scan, and a tissue sample (if surgery is done) help to focus the search for the primary disease site and to guide treatment. With the advances in the genetic profling of cancers, we are often able to determine the primary cancer resulting in metastatic brain tumor. The metastatic brain tumor usually contains the same type of cancer cells found at the primary site. For example, small-cell lung cancer metastatic to the brain forms small-cell cancer in the brain. However, recent research is suggesting that some of the tumors develop or acquire new genetic alterations in the primary tumor when they spread to the brain. These numbers are based on data reported by individual hospitals, estimates from a few individual city-based statistics and observations from autopsy results. The American Brain Tumor Association has funded research into the incidence and prevalence of these tumors. Cancer cells, visible under a microscope and detectable by a technique called fow cytometry, separate from the primary tumor and enter the circulatory (blood) system. Scientists believe circulating tumor cells use the bloodstream or lymph system for access to other organs, initially migrate and enter the lungs, then move on to other organs and in particular, the brain. Research shows that these traveling cells (circulating tumor cells) exit the blood or lymphatics and enter another part of the body. In a new organ, the tumor may lie dormant or rapidly enlarge causing new symptoms referable to the new site of metastasis. The growth of metastatic tumors is often independent of the primary site of cancer from which the tumors originated. In some situations, the process of tumor spread and growth in the metastatic organ occurs rapidly. Since blood from the lungs fows directly to the brain, lung cancer is capable of quickly spreading to the brain. Sometimes, this happens so fast that the brain metastases are found before the primary lung cancer is found. Scientists also know that primary cancers tend to send cells to particular organs. It is believed these organ preferences may be caused by small attractant molecules, chemokines, that direct and guide tumor cells to the metastatic site. In other instances cancer cells may be able to adhere, or stick, only to select organs based upon adherent molecules expressed in a particular organ. While swelling around the tumor is more common, bleeding from ruptured blood vessels in the tumor occurs in a small percentage of patients. Headaches may also be caused by cystic (water flled cavities) changes in the tumor or by interruption of spinal fuid circulation in brain resulting in a condition called hydrocephalus. During normal electrical activity, the nerve cells in the brain communicate with each other through carefully controlled electric signals. During a seizure, abnormal electrical activity occurs, that may stay in a small area or spread to other areas of brain. Disturbance in the way one thinks and processes thoughts (cognition) is another common symptom of a metastatic brain tumor. Cognitive challenges might include diffculty with memory (especially short term memory) or personality and behavior changes.