Benadryl
Order genuine benadryl
The code C914 is listed as a subaddress to D594 in the causation table so this sequence is accepted allergy laryngitis treatment buy benadryl line. Code D641 (Secondary sideroblastic anemia due to disease) when reported due to conditions listed in the causation table under address code D641. Codes for Record I (a) Pneumonia J189 (b) Sideroblastic anemia D641 (c) Alcoholic cirrhosis K703 Code to K703. The code K703 is listed as a subaddress to D641 in the causation table so this sequence is accepted. Code D642 (Secondary sideroblastic anemia due to drugs or toxins) when reported due to conditions listed in the causation table under address code D642. The code Y402 is listed as a subaddress to D642 in the causation table so this sequence is accepted. The code C959 is listed as a subaddress to D690 in the causation table so this sequence is accepted. Thrombocytopenia (D696) Code D695 (Secondary thrombocytopenia) when reported due to conditions listed in the causation table under address code D695. Codes for Record I (a) Multiple hemorrhages R5800 (b) Thrombocytopenia D695 (c) Cancer lung C349 Code to C349. The code C349 is listed as a subaddress to D695 in the causation table so this sequence is accepted. Hyperparathyroidism (E213) Code E211 (Secondary hyperparathyroidism) when reported due to conditions listed in the causation table under address code E211. Codes for Record I (a) Hypercalcemia E835 (b) Hyperparathyroidism E211 (c) Cancer parathyroid gland C750 Code to C750. The code C750 is listed as a subaddress to E211 in the causation table so this sequence is accepted. Korsakov Disease, Psychosis or Syndrome (F106) Code F04 (nonalcoholic Korsakov disease) when reported due to conditions listed in the causation table under address code F04. Codes for Record I (a) Korsakoff psychosis F04 (b) Wernicke encephalopathy E512 (c) Code to E512. The code E512 is listed as a subaddress to F04 in the causation table so this sequence is accepted. Codes for Record I (a) Pneumonia J189 (b) Psychosis cerebrovascular F09 I672 (c) arteriosclerosis (d) Arteriosclerosis I709 Code to I672. The code I709 is listed as a subaddress to F09 in the causation table so this sequence is accepted. Mental Disorder (any F99) Code F069 (Organic mental disorder) When reported due to or on the same line with conditions listed in the causation table under address code F069. Codes for Record I (a) Cardiorespiratory arrest I469 (b) Heart failure I509 (c) Mental disorder F069 (d) Multiple sclerosis G35 Code to G35. The code G35 is listed as a subaddress to F069 in the causation table so this sequence is accepted. Parkinson Disease (G20) Advanced Parkinson Disease (G2000) Grave Parkinson Disease (G2000) Severe Parkinson Disease (G2000) a. Code G214 (Vascular parkinsonism) when reported due to conditions listed in the causation table under address code G214. I (a) Parkinsonism G214 (b) Arteriosclerosis I709 (c) Code to G214 (Vascular parkinsonism) when reported due to conditions listed in the causation table under G214. Code G219 (Secondary parkinsonism) when reported due to: A170-A179 B060 B949 R75 Y20-Y369 A504-A539 B200-B24 F200-F209 S000-T357 Y600-Y849 A810-A819 B261 G000-G039 T66-T876 Y850-Y872 A870-A89 B375 G041-G09 T900-T982 Y881-Y899 B003 B900 G20-G2000 T983 B010 B902 G218-G219 X50-X599 B021-B022 B91 G300-G309 X70-X84 B051 B941 I950-I959 X91-Y09 Codes for Record 1. I (a) Parkinson disease G219 (b) Tuberculous meningitis A170 (c) Code to G219 (Secondary parkinsonism) when reported due to conditions listed in the causation table under G219. When reported due to or on the same line with conditions listed in the causation table under address code I672. The code E149 is listed as a subaddress to I672 in the causation table so this sequence is accepted. When reported as causing I600-I679 I690-I698 Codes for Record I (a) Cerebral thrombosis I633 (b) Cerebral sclerosis I672 Code to I633. Code (b) as cerebrovascular atherosclerosis since reported as causing a cerebral thrombosis. The code I251 is listed as a subaddress to I429 in the causation table so this sequence is accepted. Paralysis (any G81, G82, or G83 excluding senile paralysis) Code the paralysis for decedent age 28 days and over to G80 (Infantile cerebral palsy) with appropriate fourth character: When reported due to: P000 P969 Female, 3 months Codes for Record I (a) Pneumonia 1 wk J189 (b) Paraplegia 3 mos G808 (c) Injury spinal cord since birth P115 Code to P115. Code the paraplegia to infantile cerebral palsy when reported due to a newborn condition. Code I850 (Bleeding esophageal varices): When reported due to or on same line with: Alcoholic disease classified to: F101-F109 Liver diseases classified to: B150-B199, B251, B942, K700-K769 Toxic effect of alcohol classified to: T510-T519, T97 Codes for Record I (a) Varices I859 (b) Cirrhosis of liver K746 Code to K746. The code K746 is listed as a subaddress to I859 in the causation table; therefore, this sequence is accepted. Pneumoconiosis (J64) Code J60 (Coalworker pneumoconiosis): When Occupation is reported as: Coal miner Coal worker Miner Codes for Record Occupation: Coal Miner I (a) Bronchitis J40 (b) Pneumoconiosis J60 Code to J60. Pneumoconiosis becomes coalworker pneumoconiosis when occupation is reported as coal miner. Alveolar Hemorrhage (diffused) (K088) Code R048 (Lung hemorrhage) When reported anywhere on record with: A000-J989 S017-S023 K20-Q379 S026-S028 Q390-R825 S033 R826 R827-R892 S035-S098 R893 S100-Y899 R894-R961 R98-S014 Codes for Record I (a) Respiratory Failure J969 (b) Alveolar Hemorrhage R048 Code to R048. The alveolar hemorrhage is reported on the record with a condition listed in the causation table under address R048;therefore, this sequence is accepted. Codes for Record I (a) Lung dysplasia Q336 (b) Diaphragmatic hernia Q790 (c) Code to congenital diaphragmatic hernia (Q790). The code Q790 is listed as a subaddress to Q336 in the causation tables; therefore, this sequence is accepted. The code E149 is listed as a subaddress to K746 in the causation table; therefore, this sequence is accepted. Codes for Record I (a) Biliary cirrhosis K744 (b) Carcinoma pancreas C259 (c) Code to C259. The code C259 is listed as a subaddress to K744 in the causation table; therefore, this sequence is accepted. Lupus Erythematosus (L930) Lupus (L930) Code M321 (Systemic lupus erythematosus with organ or system involvement): When reported as causing a disease of the following systems: Anemia Circulatory (including cardiovascular, lymph nodes, spleen) Gastrointestinal Musculoskeletal Respiratory Thrombocytopenia Urinary Codes for Record I (a) Nephritis N059 (b) Lupus erythematosus M321 (c) Code to M321. Lupus is reported as causing a disease of the urinary system; therefore, it is coded as systemic lupus erythematosus. Gout (M109) Code M104 (Secondary gout): When reported due to conditions listed in the causation table under address code M104. Codes for Record I (a) Perforated gastric ulcer K255 (b) Gout M104 (c) Waldenstrom macroglobulinemia C880 Code to C880. The code C880 is listed as a subaddress to M104 in the causation table; therefore, this sequence is accepted. Kyphosis (M402) Code M401 (Secondary kyphosis): When reported due to conditions listed in the causation table under address code M401. The code M479 is listed as a subaddress to M401 in the causation table; therefore, this sequence is accepted. Scoliosis (M419) Code M415 (Secondary scoliosis): When reported due to conditions listed in the causation table under address code M415. Codes for Record I (a) Pneumonia J189 (b) Scoliosis M415 (c) Progressive systemic sclerosis M340 Code to M340. The code M340 is listed as a subaddress to M415 in the causation table; therefore, this sequence is accepted. Osteonecrosis (M879) Code M873 (Secondary osteonecrosis): When reported due to conditions listed in the causation table under address code M873. Codes for Record I (a) Septicemia A419 (b) Osteonecrosis hip M873 (c) Infective myositis M600 Code to M600. The code M600 is listed as a subaddress to M873 in the causation table; therefore, this sequence is accepted. Cesarean Delivery for Inertia Uterus (O622) Hypotonic Labor (O622) Hypotonic Uterus Dysfunction (O622) Inadequate Uterus Contraction (O622) Uterine Inertia During Labor (O622) Code O621 (Secondary uterine inertia): When reported due to conditions listed in the causation table under address code O621. Codes for Record I (a) Uterine inertia O621 (b) Diabetes mellitus of pregnancy O249 Code to O249. The code O249 is listed as a subaddress to O621 in the causation table; therefore, this sequence is accepted. Brain Damage, Newborn (P112) Code P219 (Anoxic brain damage, newborn) When reported due to: A000-P029 P040-P082 P132-P158 P200-R825 R826 R827-R892 R893 R894-R961 R98 Male, 9 hours Codes for Record I (a) Brain damage P219 (b) Congenital heart disease Q249 Code to Q249. The code Q249 is listed as a subaddress to P219 in the causation table; therefore, this sequence can be accepted.
Discount 25mg benadryl
To achieve this task allergy forecast tokyo cheap benadryl on line, stroke prevention awareness must be neurological disorders: a public health approach 161 raised among health-care planners and governments. Another priority is education of the general public and health-care providers about the preventable nature of stroke, as well as about warning symptoms of the disease and the need for a rapid response. Furthermore, allocation of resources for implementation and delivery of stroke services. Finally, it is very important to establish key national institutions and organizations that would promote training and education of health professionals and dissemination of stroke relevant information. The primary focus of this international collaboration will be to harness the necessary resources for implementing existing knowledge and strategies, especially in the middle and low income countries. The purpose of this strategy is threefold: to increase awareness of stroke; to generate surveillance data on stroke; and to use such data to guide improved strategies for prevention and management of stroke (20). The Global Stroke Initiative is only possible through a strong interaction between governments, national health au thorities and society, including two major international nongovernmental organizations. Increasing awareness and advocacy among policy-makers, health-care providers and the general public of the effect of stroke on society, health-care systems, individuals and families is fundamental to improving stroke prevention and management. Advocacy and awareness are also essential for the development of sustainable and effective responses at local, district and national levels. Policy-makers need to be informed of the major public health and economic threats posed by stroke as well as the availability of cost-effective approaches to both primary and secondary prevention of stroke. Health professionals require appropriate knowledge and skills for evidence-based prevention, acute care and rehabilitation of stroke. Relevant information needs to be provided to the public about the potential for modifying personal risk of strokes, the warning signs of impending strokes, and the need to seek medical advice in a timely manner. One of the major prob lems of stroke epidemiology is the lack of good-quality epidemiological studies in developing countries, where most strokes occur and resources are limited. This flexible and sustainable system includes three steps: standard data acquisition (recording of hospital admission rates for stroke), expanded population coverage (calculation of mortality rates by the use of death certifi cates or verbal autopsy), and comprehensive population-based studies (reports of nonfatal events to calculate incidence and case-fatality). These steps could provide vital basic epidemiological estimates of the burden of stroke in many countries around the world (20). Primary prevention of ischemic stroke: a guideline from the American Heart Association/ American Stroke Association Stroke Council. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Mortality by cause for eight regions of the world: global burden of disease study. Treatment and secondary prevention of stroke: evidence, costs, and effects on individuals and populations. Prevention of recurrent heart attacks and strokes in low and middle income populations: evidence-based recommendations for policy-makers and health professionals. Recent advances in management of transient ischaemic attacks and minor ischaemic strokes. Guidelines for prevention of stroke in patients with ischaemic stroke or transient ischaemic attack. Rehabilitation, prevention and management of complications, and dis charge planning. Many years of productive life 173 Conclusions and recommendations are lost, and many people have to suffer years of disability after brain injury. In addition, it engen ders great economic costs for individuals, families and society. The world is facing a silent epidemic of road traffic accidents in the developing countries: by 2020, road traffic crashes will have moved from ninth to third place in the world ranking of the burden of disease and will be in second place in developing countries. Systematic triage of patients can lead to important economic savings and better use of scant hospital resources. More standardized pre-hospital and in-hospital care, to minimize secondary brain injury, can improve outcomes substantially. Acceleration and deceleration forces may disrupt the nervous tissue and blood vessels of the brain. The intermediate category, “moderate” head injury, implies a mortality rate of 2–5%. Further classification of the brain injury is made in order to evaluate prognosis, identify pa tients at risk for deterioration and choose appropriate observation and treatment. Someone who opens his eyes only after painful stimulation, utters only incomprehensible sounds and withdraws his hand only after pinching will be given a score of 8. A fracture detected on the skull X-ray images indicates an increased risk of deterioration, and the patient will need admission. In spite of these reservations, it can be interesting and informative to compile data from different parts of the world. Some of the differences could be as cribed to variations in study years, inclusion criteria and research methods. Therefore, incidence rates such as 546 per 100 000 per year in Sweden and 91 per 100 000 per year in Spain must be interpreted with caution. Data from many parts of the world consistently show a peak incidence rate in children, young adults and elderly people. Information on how sequelae develop (diminish or increase) over time is scarce (8); better data on prevalence would certainly be useful for improved planning of rehabilitation needs. The average European pre-hospital case-fatality rate was 8%, while the in-hospital rate was 3%, i. Mortality rate per 100 000 population per year is more informative than the case-fatality rate. The rate is around 10 in Scandinavia, 20 in India, 30 in the United States, 38 in China, Province of Taiwan, 81 in South Africa and 120 in Colombia (10). It has been suggested that heavy alcohol abuse may explain the persistent and high mortality rate in Finland (11). Disability Traumatic brain injury is the leading cause of disability in people under 40 years of age. Disability can be classified in a simple fashion using the Glasgow Outcome Scale (see Table 3. Most patients (90%) had sustained a mild head injury, while a few had suffered moderate (5%) or severe (3%) brain injury. Even among young patients with mild injuries and a good pre-injury status, one third failed to achieve a good recovery. Mostly, patients with severe disability will have a combined mental and physical handicap. It may be transitory, subsiding after a month or so, but may persist in many cases. The persistently vegetative patient needs artificial nutrition and hydration and will have a markedly reduced life span, i. In some cases, complicated ethical and legal discussions arise about the purpose of continuing life-sustaining treatment. These variations must be taken into account by health planners who design prevention programmes. Every day about 3000 people die and 30 000 people are seriously injured on the world’s roads, nearly half of them with head injuries. Most of the victims are from the low income or middle income countries, with pedestrians, cyclists and bus passengers bearing most of the burden (12). Fatality rates among children are six times greater in developing countries than in high income countries. Terms such as “a public health crisis” and “a neglected epidemic” have been used to describe this growing problem (13). People 70 years or older have a relatively high incidence of head injuries, and in these patients falls are the most common cause. Many factors contribute to the increased risk for falls in elderly people: gait impairment, dizziness, previous stroke, cognitive impairment, postural hypotension, poor visual acuity and multiple medication. These patients can be dismissed after a short clinical examination and adequate information, since their risk of further problems will be very low, i. Before dismissal, they deserve brief information, preferably written, about: warning signs indicating possible complications; how normal and mild symptoms are expected to develop; how to resume normal daily activities. Therefore, a closer examination may be required to identify the individuals with the highest risk of developing complications. Patients who need special attention are those with: decreasing level of consciousness; neurological deficit; epileptic seizure; deficient blood coagulation; age >60 years; alcohol abuse.
Buy benadryl 25mg fast delivery
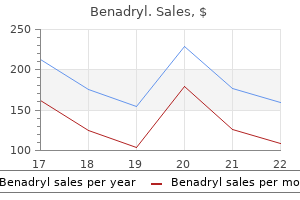
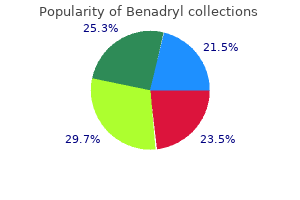
Males had a higher average number of services per patient than females (34 radiotherapy services per patient per year compared with 30) (Table 6 allergy forecast dallas order benadryl with american express. Data reported by date of service (that is, 2017 refers to services rendered between 1 January 2017 and 31 December 2017) for all services processed up to 31 August 2018. Patient numbers based on a count of unique patients who received at least 1 radiotherapy service in each calendar year. Beneft per patient is the average Medicare-subsidised radiotherapy beneft subsidised per patient. Around 90% of radiotherapy patients are over 50 In 2017, around 9 of every 10 patients receiving Medicare-subsidised radiotherapy services were over the age of 50. The youngest (0–4 years) and oldest (85 years and older) age groups had the fewest services 6 per patient (22 services) (online Table S6. Males aged 70 to 79 receive the greatest number of radiotherapy services per patient For age groups 65 and older, more males received Medicare-subsidised radiotherapy services than females (Figure 6. This may be partly attributed to the high prostate cancer incidence rate among males within this age group. Between the ages of 25 and 64, more females received radiotherapy services than males (Figure 6. This may be partly attributed to the high breast cancer incidence rate among females within this age group. Women aged between 30 and 49 received, on average, 35 Medicare-subsidised radiotherapy services and this is more than any other female age group. Men aged between 70 and 79, on average, received more Medicare-subsidised radiotherapy services than any other female or male age group. Patient numbers based on a count of unique patients who received at least 1 radiotherapy service in the calendar year. Data reported by date of service (that is, 2017 refers to services rendered between 1 January 2017 and 31 December 2017) for all services processed until 31 August 2019. Services per patient is the average number of Medicare-subsidised radiotherapy services received per patient. The principal diagnosis is the diagnosis established after study to be chiefy responsible for causing a patient’s need for the current course of treatment. Data reported for principal diagnosis may not refect the incidence of certain cancers in the Australian population. The diferences in principal diagnosis activity in this report may indicate data quality issues; for example, where some providers may be reporting the primary site of the cancer, rather than the diagnosis code associated with the health condition being treated in the specifc course of radiotherapy. Of these, around one-quarter of the radiotherapy courses for males were for prostate cancer (26%) and 44% of radiotherapy courses for females were for breast cancer. Lung cancer was the second most common reason for a radiotherapy course in both males and females (Table 6. While palliative care is provided in other settings (for example, community-based palliative care services), comprehensive national information on palliative care provided in these settings does not currently exist. Available data suggest that just over half of palliative care episodes in Australia occur in admitted patient care settings (Connolly et al. This section presents a summary of cancer-related hospitalisations where palliative care was provided within an admitted patient setting. Cancer-related hospitalisations where palliative care was provided are defned as those where. In 2016–17, 77,369 cancer-related hospitalisations in Australia involved palliative care (0. For most of these hospitalisations, the care type was recorded as palliative care (72%). For the remainder, palliative care was recorded as an additional diagnosis and provided as part of the hospitalisation where the intended care type was acute care or Cancer in Australia 2019 71 other modes of care. The most common type of cancer recorded for palliative care hospitalisation was secondary site cancer (21%), followed by lung cancer (13%) and colorectal cancer (7%) (Table 6. In 2016–17, 51% of cancer-related hospitalisations involving palliative care ended in death, 12% were transferred to another facility and 32% were discharged to where they usually live, which could be a person’s own home or welfare institution. Survival and survivorship after a cancer diagnosis 7 Key fndings In 2011–2015 in Australia. Between 1986–1990 and 2011–2015, 5-year relative survival for all cancers combined increased from 50% to 69%. Relative survival refers to the probability of being alive for a given amount of time after diagnosis compared with the general population. Information on survival from cancer provides an indication of cancer prognosis and the efectiveness of treatments available. A range of factors infuence survival from cancer, including characteristics of the patient (such as age, sex and genetics), the nature of the tumour (such as site, stage at diagnosis and histology type) and the health-care system (such as the availability of health-care services, screening, diagnostic and treatment facilities, and follow-up services) (Black et al. Survival estimates are based on the survival experience of people who were diagnosed before or during this period, and who were at risk of dying during this period. Note that the period method is an alternative to the traditional cohort method, which focuses on a group of people diagnosed with cancer in a past time period, and follows these people over time. By its nature, the period method produces more up-to-date estimates of survival than the cohort method. In this chapter, all year spans presented were calculated using the period method. All cancers combined In 2011–2015, 5-year relative survival was 69% for all cancers combined. This means that people diagnosed with cancer had a 69% chance of surviving for at least 5 years compared with their counterparts in the general population. Cancer in Australia 2019 75 Cancer survival rates are similar for males and females in younger age groups but difer for ages over 35 Up to the age of 34, males and females had similar 5-year relative survival with the exception of the 15–19 age group, where female rates were higher (90% compared with 85%). Males had higher 5-year relative survival than females for ages 65 and up (online Table S7. The diference in the age-related pattern of survival by sex may be partly due to the age distributions and survival outcomes for prostate cancer and breast cancer. For all cancers combined, 5-year survival for males increased from 45% in 1986–1990 to 68% in 2011–2015, and for females it increased from 56% to 70%. These gains may be due to better diagnostic methods, earlier detection and improvements in treatment (Dickman & Adami 2006). The cancers where females had higher rates of survival and the diferences between males and females were greatest were anal cancer (73% compared with 62%), non-melanoma of the skin (77% compared with 67%) and mouth cancer (65% compared with 57%). In 2011–2015, males had higher 5-year relative survival rates than females for bladder cancer (56% compared with 46%), cancer of unknown primary site (17% compared with 9. In the same period, 4 of the 10 most commonly diagnosed cancers for males recorded 5-year survival rates above 70%; for females 6 of the 10 most commonly diagnosed cancers recorded 5-year survival rates above 70%. The most commonly diagnosed cancer for males had a 5-year survival rate of 95% (prostate cancer); for females the most commonly diagnosed cancer (breast cancer) also had a 5-year survival rate above 90% (91%) (Table 7. For most cancers, survival rates are generally lower in the older age groups In 2011–2015, the 5-year relative survival rates for colorectal cancer, melanoma of the skin and prostate cancer did not vary considerably for those aged between 25 and 69, but rates dropped to varying extents for those aged 70 and over. For many individual cancer types, 5-year relative survival decreased with increasing age; however, the pattern of decline varied across cancer types (online Table S7. Cancer in Australia 2019 79 Spotlight on 5-year relative survival by age for cancers increasing at the greatest rate (incidence) Online Table S7. Only 1 of these cancers is a low-survival cancer (liver cancer) and 2 of the cancers have survival rates over 90% (thyroid cancer and melanoma of the skin) (online Table S7. Each of the selected cancers follows a similar general trend of higher survival rates for younger ages. The cancers with higher overall survival rates maintain higher survival rates for more ages before a decrease in the later age groups. Where 5-year relative survival rates are not presented by age, the rates cannot be released due to the small number of cases. The isolated value in the 0-4 age group relates to liver cancer, survival rates for liver cancer between the ages of 5 to 34 cannot be released due to the small number of cases. Thyroid cancer had high survival rates for most age groups up to 70–74 before a moderate decrease for those aged 75 and over.
Benadryl 25 mg on-line
Combination therapy is considered not medically necessary for individuals with low-risk disease allergy symptoms hives buy benadryl 25mg low price. Ultrahypofractionation was defined as a radiation fraction size greater or equal to 500 cGy. For an individual with localized prostate cancer who declines active surveillance, an individual with intermediate-risk prostate cancer, or an individual with high-risk prostate cancer in whom the pelvic lymph nodes are not being treated, hypofractionation radiation therapy received a strong recommendation based on high quality evidence. The recommendation was made regardless of whether the seminal vesicles are included in the treatment field, patient age, comorbidities, anatomy, and/or urinary function. Regimens of 6000 cGy in 30 radiation treatment fractions and 7000 cGy in 28 radiation treatment fractions are suggested by the guideline based on their review of the largest database. In men with low-risk prostate cancer who declined active surveillance, ultrahypofractionation was suggested as an alternative to conventional fractionation with a conditional recommendation based on a moderate quality of evidence. Page 199 of 263 Postoperative radiation therapy In the setting of postoperative prostate cancer, external beam photon radiation therapy may be beneficial in the setting of positive margins, extracapsular extension, seminal vesicle involvement, lymph node involvement, or prostate cut-through. CyberKnife stereotactic radiotherapy as monotherapy for low to intermediate-stage prostate cancer: early experience, feasibility, and tolerance. Phase I dose-escalation study of stereotactic body radiation therapy for low and intermediate-risk prostate cancer. Tumor control outcomes of patients treated with trimodality therapy for locally advanced prostate cancer. Determinants of prostate cancer-specific survival after radiation therapy for patients with clinically localized prostate cancer J Clin Oncol. Stereotactic body radiotherapy: an emerging treatment approach for localized prostate cancer. Prospective evaluation of stereotactic body radiotherapy for low and intermediate-risk prostate cancer: emulating high-dose-rate brachytherapy dose distribution. Dose gradient near target–normal structure interface for nonisocentric CyberKnife and isocentric intensity-modulated body radiotherapy for prostate cancer. Stereotactic body radiotherapy with or without external beam radiation as treatment for organ confined high-risk prostate carcinoma: a six year study. Quality of life and efficacy for stereotactic body radiotherapy for treatment of organ confined prostate cancer. The early result of whole pelvic radiotherapy and stereotactic body radiotherapy boost for high-risk localized prostate cancer. Dose escalation using conformal high-dose-rate brachytherapy improves outcome in unfavorable prostate cancer. Conformal high dose rate brachytherapy improves biochemical control and cause specific survival in patients with prostate cancer and poor prognostic factors. Stereotactic radiotherapy for organ-confined prostate cancer: early toxicity and quality of life outcomes from a multi-institutional trial. Postoperative radiation therapy after radical prostatectomy for prostate carcinoma. Analysis of potential cost benefits using reported hypofractionated radiation therapy regimens in prostate cancer in the United States. Acute toxicity after Cyberknife-delivered hypofractionated radiotherapy for treatment of prostate cancer. Sexual function after stereotactic body radiotherapy for prostate cancer: results of a prospective clinical trial. External beam radiation treatment planning for clinically localized prostate cancer. Other transabdominal approaches include low anterior resections, total mesorectal excisions, and abdominal perineal resections. The German Rectal Cancer Study Group investigated preoperative chemoradiation compared with postoperative therapy. The rectum extends from the transitional zone of the dentate line to the sigmoid colon. Individuals with isolated pelvic or anastomotic recurrence who have not received prior radiation may be appropriately treated with preoperative or postoperative chemoradiation with or without intraoperative external beam photon radiation therapy or with primary chemoradiation if deemed unresectable. External beam photon radiation therapy treatment techniques and schedules for the treatment of rectal cancer A. For unresectable cancers or individuals who are medically inoperable, doses higher than 54 Gy may be appropriate. Overview In the United States, the incidence of skin cancers outnumbers all other cancers combined, and basal cell cancers are twice as common as squamous cell skin cancers. Both types tend to occur in skin exposed to sunlight, and share the head and neck region as the area having the greatest risk for recurrence. Both occur more frequently and be more aggressive in immunocompromised transplant patients. In general, it is the squamous cell cancers that tend to be more aggressive, with a greater propensity to metastasize or to recur locoregionally. Anatomic location plays a role in risk stratification and is broken down into: "L" areas (trunk and extremities, excluding pretibia, hands, feet, nail units, ankles); "M" areas (cheeks, forehead, scalp, neck, pretibial); "H" areas (mask areas of face, including central face, eyelids, eyebrows, periorbital skin, lips, chin, overlying mandible, preauricular and postauricular skin, temple, ears, genitalia, hands, feet). Factors identified as placing the patient at increased risk for recurrence for basal and squamous cell skin cancers are included in Table 1. Management Treatment should be customized, taking into account specific factors and also patient preferences. Radiation therapy may be selected when cosmetic or functional outcome with surgery is expected to be inferior. Photon and/or electron beam techniques are medically necessary for the treatment of basal cell and squamous cell cancers of the skin for any of the following: a. Adequate surgical margins have not been achieved and further resection is not possible c. Definitive management of large cancers as an alternative to major resection requiring significant plastic repair d. Definitive, preoperative, or postoperative adjuvant therapy for a cancers at risk for local or regional recurrence due to perineural, lymphovascular invasion, and/or metastatic adenopathy f. Higher-energy external electron beam teletherapy (4 megaelectron volt [MeV] and greater) is most commonly utilized to treat the majority of localized lesions. Photon external beam teletherapy is required in circumstances in which other beams of lower energy are inadequate to reach the target depth. Treatment schedules with photons and/or electrons should be matched to the clinical circumstance, including size and depth of the lesion, histology, cosmetic goal, and risk of damage to underlying structures. Radiation doses typically range from 35 Gy in fractions of 7 Gy over 5 days, to 66 Gy in 33 fractions of 2 Gy over six and one-half weeks. The radiation prescription is to be made by a qualified radiation oncologist who is familiar with the nuances of the dose deposition that accompany the physical characteristics of the radiation beams and techniques. Dose prescription for electrons is at the 90% isodose line, and for superficial or orthovoltage radiation at the Dmax. Medical review will be required for those cases in which sequential Page 209 of 263 treatment is requested, or if a new request is received for treatment of additional skin cancers within 90 days of previous requests. Overview Malignant melanoma is increasing in incidence in the United States at a rate more rapidly for men than any other malignancy, and more rapidly for women for all malignancies except lung cancer. The incidence may be even higher, skewed by under-reporting of superficial and in situ cases. Some cases of melanoma take an indolent course while others are biologically much more aggressive. There are specific genetic alterations in distinct clinical subtypes of melanoma, often correlated with degree of sun damage. The risk of all three may be greater than that of a non-melanoma skin cancer in the same location. A preoperative evaluation should include a careful physical examination of the primary site, the regional lymphatics, and the entire skin surface. Equivocal findings on physical examination of the regional lymphatics may trigger an ultrasound exam of the area. The optimal degree of clear margin necessary to minimize the risk of local is dependent on tumor thickness. Lentigo maligna and melanoma in situ present unique features because of possible lateral subclinical extension, for which imiquimod is an option. Radiation therapy has been also used in such cases, with complete clearance rates in the 85% to 90% range. Radiation therapy is one option for the treatment of in-transit disease (metastases within lymphatics or satellite locations without metastatic nodes) for which resection is not feasible. Alternatives include intralesional injections, local ablation therapy, and topical imiquimod.
Purchase benadryl 25 mg fast delivery
Rechallenge with a single medicine or sequential rechallenge with both medicines after recovery may be considered allergy to cold cheap benadryl amex. Special populations Elderly No dose adjustment is necessary in patients ≥ 65 years (see section 5. For instructions on reconstitution and dilution of the medicinal product before administration, see section 6. Most immune-related adverse reactions occurring during treatment with pembrolizumab were reversible and managed with interruptions of pembrolizumab, administration of corticosteroids and/or supportive care. Immune-related adverse reactions affecting more than one body system can occur simultaneously. For suspected immune-related adverse reactions, adequate evaluation to confirm aetiology or exclude other causes should be ensured. Based on the severity of the adverse reaction, pembrolizumab should be withheld and corticosteroids administered. Immune-related pneumonitis Pneumonitis has been reported in patients receiving pembrolizumab (see section 4. Suspected pneumonitis should be confirmed with radiographic imaging and other causes excluded. Corticosteroids should be administered for 6 Grade ≥ 2 events (initial dose of 1-2 mg/kg/day prednisone or equivalent followed by a taper); pembrolizumab should be withheld for Grade 2 pneumonitis, and permanently discontinued for Grade 3, Grade 4 or recurrent Grade 2 pneumonitis (see section 4. Immune-related colitis Colitis has been reported in patients receiving pembrolizumab (see section 4. Corticosteroids should be administered for Grade ≥ 2 events (initial dose of 1-2 mg/kg/day prednisone or equivalent followed by a taper); pembrolizumab should be withheld for Grade 2 or Grade 3 colitis, and permanently discontinued for Grade 4 or recurrent Grade 3 colitis (see section 4. The potential risk of gastrointestinal perforation should be taken into consideration. Immune-related hepatitis Hepatitis has been reported in patients receiving pembrolizumab (see section 4. Immune-related nephritis Nephritis has been reported in patients receiving pembrolizumab (see section 4. Immune-related endocrinopathies Severe endocrinopathies, including adrenal insufficiency, hypophysitis, type 1 diabetes mellitus, diabetic ketoacidosis, hypothyroidism, and hyperthyroidism have been observed with pembrolizumab treatment. Corticosteroids to treat adrenal insufficiency and other hormone replacement should be administered as clinically indicated. Pembrolizumab should be withheld or discontinued for Grades 3 or 4 adrenal insufficiency or hypophysitis. Continuation of pembrolizumab may be considered, after corticosteroid taper, if needed (see section 4. Type 1 diabetes mellitus, including diabetic ketoacidosis, has been reported in patients receiving pembrolizumab (see section 4. Patients should be monitored for hyperglycaemia or other signs and symptoms of diabetes. Insulin should be administered for type 1 diabetes, and pembrolizumab should be withheld in cases of type 1 diabetes associated with Grade ≥ 3 hyperglycaemia or ketoacidosis until metabolic control is achieved (see section 4. Hypothyroidism may be managed with replacement therapy without treatment interruption and 7 without corticosteroids. Pembrolizumab should be withheld for Grade ≥ 3 until recovery to Grade ≤ 1 hyperthyroidism. Immune-related skin adverse reactions Immune-related severe skin reactions have been reported in patients receiving pembrolizumab (see section 4. Based on the severity of the adverse reaction, pembrolizumab should be withheld for Grade 3 skin reactions until recovery to Grade ≤ 1 or permanently discontinued for Grade 4 skin reactions, and corticosteroids should be administered (see section 4. Caution should be used when considering the use of pembrolizumab in a patient who has previously experienced a severe or life-threatening skin adverse reaction on prior treatment with other immune-stimulatory anticancer agents. Other immune-related adverse reactions the following additional clinically significant, immune-related adverse reactions have been reported in clinical studies or in post-marketing experience: uveitis, arthritis, myositis, myocarditis, pancreatitis, Guillain-Barré syndrome, myasthenic syndrome, haemolytic anaemia, sarcoidosis and encephalitis (see sections 4. Pembrolizumab must be permanently discontinued for any Grade 3 immune-related adverse reaction that recurs and for any Grade 4 immune-related adverse reaction. Treatment with pembrolizumab may increase the risk of rejection in solid organ transplant recipients. The benefit of treatment with pembrolizumab versus the risk of possible organ rejection should be considered in these patients. Patients with Grades 1 or 2 infusion reaction may continue to receive pembrolizumab with close monitoring; premedication with antipyretic and antihistamine may be considered. Factors associated with early deaths were fast progressive disease on prior platinum therapy and liver metastases. For patients ≥ 75 years, pembrolizumab combination therapy should be used with caution after careful consideration of the potential benefit/risk on an individual basis (see section 5. Liver enzymes should be monitored before initiation of and periodically throughout treatment. Patients with active infections occurring during treatment with pembrolizumab were managed with appropriate medical therapy. After careful consideration of the potential increased risk, pembrolizumab may be used with appropriate medical management in these patients. Since pembrolizumab is cleared from the circulation through catabolism, no metabolic drug-drug interactions are expected. Corticosteroids can also be used as premedication, when pembrolizumab is used in combination with chemotherapy, as antiemetic prophylaxis and/or to alleviate chemotherapy-related adverse reactions. These results indicate a potential risk, based on its mechanism of action, that administration of pembrolizumab during pregnancy could cause foetal harm, including increased rates of abortion or stillbirth. Human immunoglobulins G4 (IgG4) are known to cross the placental barrier; therefore, being an IgG4, pembrolizumab has the potential to be transmitted from the mother to the developing foetus. There were no notable effects in the male and female reproductive organs in monkeys based on 1-month and 6-month repeat dose toxicity studies (see section 5. The frequencies included below and in Table 2 are based on all reported adverse drug reactions, regardless of the investigator assessment of causality. In this patient population, the most frequent adverse reactions were anaemia (50%), nausea (50%), fatigue (37%), constipation (35%), diarrhoea (30%), neutropaenia (30%), decreased appetite (28%) and vomiting (25%). Adverse reactions known to occur with pembrolizumab or chemotherapies given alone may occur during treatment with these medicinal products in combination, even if these reactions were not reported in clinical studies with combination therapy. Frequencies are defined as: very common (≥ 1/10); common (≥ 1/100 to < 1/10); uncommon (≥ 1/1,000 to < 1/100); rare (≥ 1/10,000 to < 1/1,000); very rare (< 1/10,000); and not known (cannot be estimated from the available data). Within each frequency grouping, adverse reactions are presented in the order of decreasing seriousness. Table 2: Adverse reactions in patients treated with pembrolizumab* Monotherapy Combination with Combination with chemotherapy axitinib Infections and infestations Common pneumonia pneumonia pneumonia Blood and lymphatic system disorders Very common anaemia anaemia, neutropaenia, thrombocytopaenia Common thrombocytopaenia, febrile neutropaenia, anaemia, neutropaenia, lymphopaenia leukopaenia, leukopaenia, lymphopaenia thrombocytopaenia Uncommon neutropaenia, leukopaenia, lymphopaenia, eosinophilia eosinophilia Rare immune thrombocytopenic eosinophilia purpura, haemolytic anaemia, pure red cell aplasia, haemophagocytic lymphohistiocytosis Immune system disorders a a Common infusion related reaction infusion related reaction infusion related a reaction Uncommon sarcoidosis Not known solid organ transplant rejection Endocrine disorders b Very common hypothyroidism hyperthyroidism, b hypothyroidism d Common hyperthyroidism hypothyroidism, hypophysitis, e hyperthyroidism thyroiditis, adrenal c insufficiency c d Uncommon adrenal insufficiency, hypophysitis, d e e hypophysitis, thyroiditis thyroiditis, adrenal c insufficiency 12 Metabolism and nutrition disorders Very common decreased appetite hypokalaemia, decreased decreased appetite appetite Common hyponatraemia, hyponatraemia, hypokalaemia, hypokalaemia, hypocalcaemia hyponatraemia, hypocalcaemia hypocalcaemia f f Uncommon type 1 diabetes mellitus type 1 diabetes mellitus type 1 diabetes mellitus Psychiatric disorders Common insomnia insomnia insomnia Nervous system disorders Very common headache dizziness, headache, headache, dysgeusia neuropathy peripheral, dysgeusia Common dizziness, neuropathy lethargy dizziness, lethargy, peripheral, lethargy, neuropathy peripheral dysgeusia h Uncommon epilepsy epilepsy myasthenic syndrome g Rare Guillain-Barré syndrome, h myasthenic syndrome, i meningitis (aseptic), encephalitis Eye disorders Common dry eye dry eye dry eye j j Uncommon uveitis uveitis Rare Vogt-Koyanagi-Harada syndrome Cardiac disorders † † † Common cardiac arrhythmia cardiac arrhythmia cardiac arrhythmia (including atrial (including atrial (including atrial fibrillation) fibrillation) fibrillation) k Uncommon pericardial effusion, pericardial effusion myocarditis pericarditis k k Rare myocarditis myocarditis, pericarditis Vascular disorders Very common hypertension Common hypertension hypertension Respiratory, thoracic and mediastinal disorders Very common dyspnoea, cough dyspnoea, cough dyspnoea, cough, dysphonia l l l Common pneumonitis pneumonitis pneumonitis Gastrointestinal disorders Very common diarrhoea, abdominal diarrhoea, nausea, diarrhoea, abdominal m m pain, nausea, vomiting, vomiting, constipation, pain, nausea, vomiting, m constipation abdominal pain constipation n n n Common colitis, dry mouth colitis, dry mouth colitis, dry mouth o o o Uncommon pancreatitis pancreatitis pancreatitis Rare small intestinal perforation Hepatobiliary disorders p Common hepatitis p p Uncommon hepatitis hepatitis Skin and subcutaneous tissue disorders q r q r Very common rash, pruritus rash, alopecia, pruritus palmar-plantar erythrodysaesthesia q syndrome, rash, r pruritus 13 s s s Common severe skin reactions, severe skin reactions, severe skin reactions, erythema, dry skin, erythema, dry skin dermatitis acneiform, t vitiligo, eczema, alopecia, dermatitis, dry skin, dermatitis acneiform alopecia, eczema, erythema u Uncommon lichenoid keratosis, psoriasis, dermatitis hair colour changes, psoriasis, dermatitis, acneiform, dermatitis, lichenoid keratosis, t papule, hair colour changes vitiligo, eczema papule, psoriasis, t vitiligo Rare toxic epidermal necrolysis, hair colour changes, Stevens-Johnson syndrome, lichenoid keratosis, erythema nodosum papule Musculoskeletal and connective tissue disorders v v v Very common musculoskeletal pain, musculoskeletal pain, musculoskeletal pain, arthralgia arthralgia arthralgia, pain in extremity w w x Common pain in extremity, myositis, pain in myositis, arthritis, w x x y myositis, arthritis extremity, arthritis tenosynovitis y y Uncommon tenosynovitis tenosynovitis Renal and urinary disorders z Common nephritis, acute kidney acute kidney injury, z injury nephritis z Uncommon nephritis General disorders and administration site conditions aa Very common fatigue, asthenia, oedema, fatigue, asthenia, pyrexia, fatigue, asthenia, aa pyrexia oedema pyrexia aa Common influenza-like illness, chills chills, influenza-like oedema, influenza-like illness illness, chills Investigations Very common blood creatinine alanine increased aminotransferase increased, aspartate aminotransferase increased, blood creatinine increased Common aspartate aminotransferase hypercalcaemia, alanine blood alkaline increased, alanine aminotransferase phosphatase increased, aminotransferase increased, increased, aspartate hypercalcaemia, blood hypercalcaemia, blood aminotransferase bilirubin increased alkaline phosphatase increased, blood alkaline increased, blood bilirubin phosphatase increased increased, blood creatinine increased Uncommon amylase increased blood bilirubin increased, amylase increased amylase increased *Adverse reaction frequencies presented in Table 2 may not be fully attributable to pembrolizumab alone but may contain contributions from the underlying disease or from other medicinal products used in a combination. Immune-related skin adverse reactions Immune-related severe skin reactions occurred in 89 (1. Of the patients who recovered, 92 (84%) were rechallenged with either pembrolizumab (3%) or axitinib (31%) monotherapy or with both (50%). Laboratory abnormalities In patients treated with pembrolizumab monotherapy, the proportion of patients who experienced a shift from baseline to a Grade 3 or 4 laboratory abnormality was as follows: 10. Immunogenicity In clinical studies in patients treated with pembrolizumab 2 mg/kg every three weeks, 200 mg every three weeks, or 10 mg/kg every two or three weeks as monotherapy, 36 (1. There was no evidence of an altered pharmacokinetic or safety profile with anti-pembrolizumab binding or neutralising antibody development. The most common adverse reactions (reported in at least 20% of paediatric patients) were pyrexia (31%), 17 vomiting (26%), headache (22%), abdominal pain (21%), anaemia (21%) and constipation (20%). The majority of adverse reactions reported for monotherapy were of Grades 1 or 2 severity. It allows continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are asked to report any suspected adverse reactions via the national reporting system listed in Appendix V. In case of overdose, patients must be closely monitored for signs or symptoms of adverse reactions, and appropriate symptomatic treatment instituted. Based on the modelling and simulation of dose/exposure relationships for efficacy and safety for pembrolizumab, there are no clinically significant differences in efficacy or safety among the doses of 200 mg every 3 weeks, 2 mg/kg every 3 weeks, and 400 mg every 6 weeks as monotherapy (see section 4. Sixty-five percent of patients had M1c stage, 9% had a history of brain metastases, 66% had no and 34% had one prior therapy. Table 3 summarises key efficacy measures in patients naïve to treatment with ipilimumab at the final analysis performed after a minimum of 21 months of follow-up. Patients were treated with pembrolizumab until disease progression or unacceptable toxicity.
Order benadryl on line
The main objective of patient transfers is to ensure patients are safe to reach the destination in the most appropriate time allergy vs sensitivity benadryl 25mg amex. The criteria for the mode and rapidity of transferring patients with head injury in the pre-hospital setting are based on the risk of intracranial complications and severity of head injury. Alternatively patients can be directly transported to a centre capable to initially manage their condition. Cervical spine immobilisation should be maintained during transfer until a full assessment and appropriate investigations are performed. The referring health care providers should determine whether an ambulance or other mode of medical transport is required. Public transport and car are appropriate alternative means provided the patients are accompanied. The risk of secondary brain injury during transfer to tertiary centre is high if poorly executed. Recommendation 5 Triage of patients suspected of head injury in pre-hospital care or on arrival in emergency department should follow a four-step algorithm* based on physiologic abnormalities, anatomic injuries, mechanism of injuries and co-morbidities and age. However they usually require further observation after initial systematic assessment and treatment. The primary aim is to detect promptly patients who deteriorate neurologically and to ensure safe home discharge. Early imaging, rather than admission and observation for neurological deterioration, will reduce the time to detection for life-threatening complications and is associated with better Fabrri A et al. Frequency Frequency of observation should relate to risk of clinically important findings in order to detect early deterioration of head injury. The risk of rapid deterioration due to intracranial complications is high during the first six hours and diminishes after that. Some clinical risk factors can be used as a guide to identify those who need neurosurgical intervention. Recommendation in this section is formulated based on extrapolation from other guidelines and tailored to local context. Recommendation 11 Patient with low risk mild head injury* can be discharged safely without observation from emergency department or primary care with reliable care giver. Early imaging prevents deterioration of patients’ condition due to expansion of intracranial lesions and expedites appropriate surgical and medical interventions. Scandinavian Neurotrauma Committee has concluded that the presence of the following Undén J et al. Intracranial haemorrhage cannot cause haemorrhagic shock, except in the terminal stages when medullary failure supervenes or there is a concomitant spinal cord injury. The scan is indicated when there is anatomical and/or physiological evidence of head injury. In the absence of clinical signs of skull fracture, one cannot rule out the presence of skull fracture. Sensitivity and specificity of clinical assessment on skull fracture Clinical findings Sensitivity Specificity Clinical assessment (both clinical signs of 51. A Cochrane systematic review revealed no significance in mortality and severe disability between barbiturate and control group. There is no retrieval evidence on the use of analgesia/sedation/reversal in mild to moderate head injury. Brain Injury Special Interest Group of the American Academy of Physical Medicine and this can prevent secondary brain injury. There is no significant difference between levetiracetam and phenytoin with regards to seizure rate, adverse drug reaction, complication and mortality. It is also not significantly associated with progression of injury based on imaging. Recommendation 17 Early extracranial surgery in head injury patients can be performed safely under general anaesthesia. Extubation of these patients demands consideration of airway patency, respiratory parameters, neurological status and associated injury. Points to be considered include timing and place of extubation, and post-extubation care. In view of limited evidence, the following points are to be considered prior to extubation. It Stormo A et changes the treatment at the referring hospital on the advice of the neurosurgeon (42%). Recommendation 18 Teleconsultation should be used in the management of head injury if available. This will help them to identify alarming features that need immediate medical Kerr J et al. I the discharge form should include facilities contact details in the event of emergency or Fung M et al. Therefore a discharge form should be standardised and comprehensible at all levels. Recommendation 20 Moderate to severe head injury should have scheduled clinic follow-up. Medical outcome after immediate computed tomography or admission for observation in patients with mild head injury: randomised controlled trial. Pre-hospital care management of a potential spinal cord injured patient: a systematic review of the literature and evidence based guidelines. The value of scheduled repeat cranial computed tomography after mild head injury: single-center series and meta-analysis. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Prehospital hypertension is predictive of traumatic brain injury and is associated with higher mortality. The relationship between pre-hospital and emergency department Glasgow coma scale scores. Treatments for reversing warfarin anticoagulation in patients with acute intracranial hemorrhage: a structured literature review. Incidence and predictors of intracranial hemorrhage after minor head trauma in patients taking anticoagulant and antiplatelet medication. Guidelines for the management of 30 spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Chan Chi Ho Clinical predictors of minor head injury patients presenting with Glasgow Coma Scale score of 14 or 15 and requiring neurosurgical intervention Hong Kong j. Restarting anticoagulation therapy after warfarin-associated intracerebral hemorrhage. Clinical Features of Head Injury Patients Presenting With a Glasgow Coma Scale Score of 15 and Who Require Neurosurgical Intervention. Canadian Cervical Spine rule compared with computed tomography: a prospective analysis. Observational approach to subjects with mild-to moderate head injury and initial non-neurosurgical lesions. Prospective validation of a proposal for diagnosis and management of patients attending the emergency department for mild head injury. Which type of observation for patients with high risk mild head injury and negative computed tomography? Risk factors for cervical spine injury among patients with traumatic brain injury. A proposal for an evidenced-based emergency department discharge form for mild traumatic brain injury. Prophylaxis of the epilepsies: should anti-epileptic drugs be used for preventing seizures after acute brain injury? Comparison of the safety and efficacy of propofol with midazolam for sedation of patients with severe traumatic brain injury: a meta-analysis. The implementation of teleneurosurgery in the management of referrals to a neurosurgical department in hospital sultanah amninah johor bahru. Management of anticoagulation following central nervous system hemorrhage in patients with high thromboembolic risk. Health Indicators 2014: Indicators for Monitoring and Evaluation of Strategy Health for All.
Diseases
- Netherton syndrome ichthyosis
- Fascioliasis
- Ventricular extrasystoles perodactyly Robin sequence
- Amelia (birth defect)
- Rapadilino syndrome
- Coffin Siris syndrome
- TAR syndrome
- Camurati Engelmann disease
Buy cheap benadryl
No adverse clinical effects were noted in the mice for up to 6 h after drug injection egg allergy symptoms joint pain benadryl 25mg overnight delivery. We investigated whether the fast elimination could be due to enzymatic degradation using published techniques (Gynther, Laine et al. Both compounds exhibited activity in established glioma lines maintained in both serum-containing medium and as neurospheres in defined medium. They grow as neurospheres in serum-free media, and in this study, the effects of the imidazotetrazine 58 analogs on neurosphere growth were evaluated in cell line and patient-derived neurospheres. The neurosphere recovery assay provides a 3-dimensional tumor model that measures acute responses to drug therapy and the clonogenic potential of cells following treatment. The impact of drug therapy also was evaluated in neurosphere cultures derived directly from patient-derived xenograft lines. All three compounds undergo pH-dependent hydrolytic ring-opening 60 reactions to generate reactive diazonium ions. Based on these data, medicinal chemistry approaches are being used to optimize the drug-like properties 62 for improved biodistribution. Secondary anti-rabbit IgG, peroxidase-linked and anti-mouse IgG, peroxidase-linked were purchased from Cell Signaling Technologies and Pierce, respectively. All primary antibodies were incubated overnight at 4 ºC followed by room temperature incubation with a secondary antibody conjugated with horseradish peroxidase for 1 h. Detection was performed with Super Signal Chemiluminescent reagent according to the manufacturer’s protocol (Pierce). Primary spheres were counted on day 7 and cells were fed with neurosphere medium (2 mL). Spheres for the recovery phase were counted on day 14, dissociated 67 using a basic pH dissociation method (Sen, Kallos et al. Neutralization buffer was added drop-wise to the slides followed by rinsing in distilled water, fixation in 100% ice-cold ethanol and drying overnight. Tumor growth was monitored, and mice were 3 sacrificed when tumor volumes reached 1000-1200 mm. Drug was delivered on five consecutive days and drug th volumes used to treat used were based on tumor volumes (1/10 of tumor volume). Groups of 3 mice were euthanized at times up to 6 h after injection, and plasma was harvested for analysis. A is a representative of two independent experiments plated in triplicate while B-C is one experiment plated in triplicate. During the course of the assay neurospheres are quantified at day 7 (treatment phase), day 14 (recovery phase), and day 21 (secondary sphere formation phase). In this chapter, I was responsible for the majority of experimental set-up, data acquisition, and analysis. In order to design a more targeted therapy, the signaling and regulatory mechanisms which are unique to senescence need to be elucidated. The upregulation was greatest at day 21, coinciding with senescence and suggesting a role for miR-34a in inducing senescence. MiR-34a overexpression modified cell cycle profiles by inducing a G1 arrest, but apoptosis was not detected. Notch family members were investigated as potential targets of miR-34a through which these effects might be mediated. Overexpression of miR-34a reduced Notch-1, Notch-2, and Notch-3 levels in glioma cultures. One approach to overcome resistance has been to develop novel combination therapies. Notch is a promising candidate for combination therapy as it regulates proliferation, cell death, differentiation, and cancer stem cell maintenance (Lino, Merlo et al. Notch inhibition in combination with other agents is promising as inhibition of Notch sensitizes cells to radiation (Wang, Chadalavada et al. This is of interest as treatments that induce cytostasis, the inhibition of proliferation without induction of cell death, are being evaluated as novel therapies. Our data also provides evidence for the involvement of miR-34a in the regulation of the Notch pathway. MiR-519 showed no detectable transcript in these glioma lines and was not further pursued. MiR-34a transcript levels appear to correlate with the p53 status of the lines, with p53 mutant lines having low miR-34a expressions and p53 wild-type have higher expression. It has been previously shown that p53 regulates miR-34a levels (Bommer, Gerin et al. MiR-34a transfected cultures formed neurospheres with large cells in loose aggregates. A simple explorative evaluation into miR-34a effects on neurosphere self-renewal was carried out by pH dissociating spheres seven days post-transfection, 101 replating, and observing sphere formation seven days later (Figure 3. Overexpression of miR-34a did induce a slight, but statistically significant, G1 arrest in cells (Figure 3. These results suggest that miR-34a overexpression fails to induce apoptosis but does alter cell cycle progression in glioma cells. Because of this we examined whether dysregulation of miR-34a drives cells into senescence. Notch family members are negatively regulated by miR-34a In silico analysis using TargetScan (Lewis, Burge et al. We examined changes in expression of Notch receptors following miR-34a overexpression. Western analysis 103 shows that expression of miR-34a inversely correlates with the expression of Notch receptors (Figure 3. Activation of the Notch pathway occurs following the interaction of ligand on one cell with a receptor on a neighboring cell (Bray 2006). In line with this, we observed that downregulation of Notch receptors was affected by density at which assays were plated (Figure 3. The down-regulation of Notch family receptors (Notch-1, -2, and -3) by miR-34a might be one mechanism by which miR-34a exerts its tumor suppressive effects. MiR-34a was upregulated in colon cancer cell lines following Adriamycin (Tazawa, Tsuchiya et al. While the upregulation we measured is in agreement with these studies, many of those studies showed that upregulation occurred in a p53-dependent manner. Due to the large number of miR 34a targets, invasion could be regulated through many pathways. In our system, miR-34a downregulates members of the Notch family and Notch has been shown to promote invasion mediated by cross-talk with Wnt pathway proteins (Hurlbut, Kankel et al. In this study we showed Notch-1, Notch-2, and Notch-3 receptors expression is downregulated by miR-34a overexpression. However, there are no published reports of miR-34a regulating Notch-3 directly or indirectly therefore validating this target would be of interest. Similarly, Notch-3 regulation by miR-206 leads to apoptosis and decrease in migration (Song, Zhang et al. Neurospheres were dissociated every seven days via acid-base dissociation (Sen, Kallos et al. Recovery and secondary sphere assay To quantify neurospheres in a recovery and secondary sphere assay (Gilbert, Daou et al. Because clonal density has been previously defined as ≤ 10cells/ μL (Chaddah, Arntfield et al. On day 14 of the assay, spheres were dissociated using a basic pH dissociation method (Sen, Kallos et al. A non-targeting Negative Control #1 (Applied Biosystems) was used as a negative control. Initial transfection efficiencies were examined using Cy3™ Dye-Labeled Pre-miR Negative Control #1 (Ambion) (Figure 3. Monitoring Cy3 fluorescence signal allowed us to analyze transfection efficiencies.

Purchase 25mg benadryl otc
Influence of patient age on biochemical freedom from disease in patients undergoing conformal proton radiotherapy of organ-confined prostate cancer allergy symptoms in dogs eyes best purchase benadryl. Postoperative spot-scanning proton radiation therapy for chordoma and chondrosarcoma in children and adolescents: initial experience at Paul Scherrer Institute. Extracranial chordoma: outcome in patients treated with function-preserving surgery followed by spot-scanning proton beam irradiation. Imaging changes in very young children with brain tumors treated with proton therapy and chemotherapy. Reduction in patient-reported acute morbidity in prostate cancer patients treated with 81-Gy intensity-modulated radiotherapy using reduced planning target volume margins and electromagnetic tracking: assessing the impact of margin reduction study. National Council on Radiation Protection and Measurements report shows substantial medical exposure increase. Small bowel toxicity after high dose spot scanning-based proton beam therapy for paraspinal/retroperitoneal neoplasms. Value and perspectives of proton radiation therapy for limited stage prostate cancer. Second nonocular tumors among survivors of retinoblastoma treated with contemporary photon and proton radiotherapy. Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer. Advanced prostate cancer: the results of a randomized comparative trial of high dose irradiation boosting with conformal protons compared with conventional dose irradiation using photons alone. Fractionated, stereotactic proton beam treatment of cerebral arteriovenous malformations. Proton radiation for treatment of cancer of the oropharynx: early experience at Loma Linda University Medical Center using a concomitant boost technique. Quality of life in patients with chordomas/chondrosarcomas during treatment with proton beam therapy. Proton-beam therapy for hepatocellular carcinoma associated with portal vein tumor thrombosis. Acute toxicity of proton beam radiation for pediatric central nervous system malignancies. Accelerated partial breast irradiation using proton beams: initial dosimetric experience. Upper gastrointestinal complications associated with gemcitabine-concurrent proton radiotherapy for inoperable pancreatic cancer. Patient-reported long-term outcomes after conventional and high-dose combined proton and photon radiation for early prostate cancer. Analysis of the relationship between tumor dose inhomogeneity and local control in patients with skull base chordoma. Long-term follow-up of proton irradiated malignant melanoma by glucose-fructose enhanced magnetic resonance imaging. Spot-scanning proton therapy for malignant soft tissue tumors in childhood: first experiences at the Paul Scherrer Institute. Proton radiation therapy for primary sphenoid sinus malignancies: treatment outcome and prognostic factors. Accounting for range uncertainties in the optimization of intensity modulated proton therapy. Hip fractures and pain following proton therapy for management of prostate cancer. Summary of Proposed 2014 Rules for the Hospital Outpatient Prospective Payment System & Medicare Fee Schedule. Adjuvant intra-arterial hepatic fotemustine for high-risk uveal melanoma patients. Proton beam stereotactic radiosurgery for pediatric cerebral arteriovenous malformations. Proton beam radiosurgery for vestibular schwannoma: tumor control and cranial nerve toxicity. Visual outcome of accelerated fractionated radiation for advanced sinonasal malignancies employing photons/protons. Spot-scanning proton radiation therapy for recurrent, residual or untreated intracranial meningiomas. Spot scanning proton therapy in the curative treatment of adult patients with sarcoma: the Paul Scherrer Institute experience. Results of spot-scanning proton radiation therapy for chordoma and chondrosarcoma of the skull base: the Paul Scherrer Institut experience. Spot scanning-based proton therapy for intracranial meningioma: long-term results from the Paul Scherrer Institute. Benign meningioma: partially resected, biopsied, and recurrent intracranial tumors treated with combined proton and photon radiotherapy. Comparison of episcleral plaque and proton beam radiation therapy for the treatment of choroidal melanoma. Surveillance of craniopharyngioma cyst growth in children treated with proton radiotherapy. Proton radiotherapy as an alternative to extenteration in the management of extended conjunctival melanoma. Technology insight: proton beam radiotherapy for treatment in pediatric brain tumors. Standard fractionation low-dose proton radiotherapy for diffuse choroidal hemangiomas in pediatric Sturge-Weber syndrome. Proton-beam, intensity-modulated, and/or intraoperative electron radiation therapy combined with aggressive anterior surgical resection for retroperitoneal sarcomas. Proton versus intensity-modulated radiotherapy for prostate cancer: patterns of care and early toxicity. Proton beam therapy as a nonsurgical approach to mucosal melanoma of the head and neck: a pilot study. Proton beam therapy for unresectable malignancies of the nasal cavity and paranasal sinuses. Comparison of conventional-dose vs high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial. Rooted in the collaborative work of centers worldwide, the definition and grading of tumors continually evolves to reflect current findings and knowledge including incorporation of genetic profiles. The scale ranges in 10-point increments from 100 (normal activity without any special care) to 0 (dead). Intermediate points balance a patient’s care needs with his/her ability to carry out normal activities. The scale ranges from 0 (fully active) to 5 (dead) with the intermediate grades as described below. Grade 0 Fully active without restriction Grade 1 Restricted in physically strenuous activity, but ambulatory and able to carry out light housework or office work Grade 2 Ambulatory and capable of self-care, but unable to work; active for >50% of waking hours Grade 3 Limited self-care; confined to bed or chair >50% of waking hours Grade 4 Completely disabled; confined to bed or chair; incapable of self-care Grade 5 Dead Source: Péus D, Newcomb N, Hofer S. Appraisal of the Karnofsky Performance Status and proposal of a simple algorithmic system for its evaluation. Events are evaluated on a scale ranging from 0 (no change from baseline) to 5 (death) for organs or body areas impacted by therapy. Late radiation effects are similarly evaluated on a scale ranging from 0 (no effects) to 5 (death) for organs or body areas impacted by therapy. Men are asked to evaluate their experiences and symptoms over the previous 4-week period. Gleason score Following a biopsy of the prostate, cancerous tissue will be graded based on microscopic findings. The Gleason score typically ranges from 2 to 10, with higher scores indicating a greater likelihood of the cancer spreading. Gleason score Related description of findings ≤ 6 Well-differentiated, less likely to spread 7 Moderately differentiated 8 10 Poorly differentiated, more likely to spread Source: American Cancer Society. Liver Cancer Child-Pugh Classification Designed to assess the severity of liver cirrhosis on a 15-point scale, the Child-Pugh assessment is based on clinical and biochemical measurements associated with liver function. Measurements Grade of hepatic encephalopathy Ascites Total bilirubin Serum albumin Prothrombin time (sec. Author (Year) Sample Size Outcomes Inclusion/Exclusion Treatment Study Design Patient Assessed Harms Quality Notes Criteria Protocol Study Site Characteristics Main Findings No comparative studies identified Table 6. Author (Year) Sample Size Outcomes Inclusion/Exclusion Treatment Study Design Patient Assessed Harms Quality Notes Criteria Protocol Study Site Characteristics Main Findings No comparative studies identified Table 15.
Buy benadryl overnight
Effects of prophylactic chemotherapy for persistent trophoblastic disease in patients with complete hydatidiform mole allergy forecast jerusalem israel buy cheap benadryl 25mg on-line. Influence of oral contraceptives in the development of post-molar trophoblastic neoplasia-a systematic review. Combined oral contraceptive and intrauterine device use among women with gestational trophoblastic disease. Clinical management and diagnostic possibilities in hydatidiform mole with coexistent fetus. Chemotherapy and human chorionic gonadotropin concentrations 6 months after uterine evacuation of molar pregnancy: a retrospective cohort study. A comparison of patients with relapsed and chemo-refractory gestational trophoblastic neoplasia. Influence of chemotherapy for gestational trophoblastic disease on subsequent pregnancy outcome. Management of gestational trophoblastic diseases: subsequent pregnancy experience. The effect of early pregnancy following chemotherapy on disease relapse and foetal outcome in women treated for gestational trophoblastic tumours. Because each oncology case is medically unique, these guidelines recommend a patient-specific approach consisting of the following components: diagnosis, staging, therapeutic intervention, provisions for patient and personnel safety in handling chemotherapy agents, referral to an oncology specialty practice when appropriate, and a strong emphasis on client support. Determination of tumor type by histologic examination of a biopsy sample should be the basis for all subsequent steps in oncology case management. Diagnostic staging determines the extent of local disease and presence or absence of regional or distant metastasis. The choice of therapeutic modalities is based on tumor type, histologic grade, and stage, and may include surgery, radiation therapy, chemotherapy, immunotherapy, and adjunctive therapies, such as nutritional support and pain management. These guidelines discuss the strict safety precautions that should be observed in handling chemotherapy agents, which are now commonly used in veterinary oncology. Because cancer is often a disease of older pets, the time of life when the pet–owner relationship is usually strongest, a satisfying outcome for all parties involved is highly dependent on good communication between the entire healthcare team and the client, particularly when death or euthanasia of the patient is being considered. These guidelines include comprehensive tables of common canine and feline cancers as a resource for case management and a sample case history. This document is intended as a Department of Clinical Sciences, College of Veterinary Medicine, guideline only. Because each case is Errors appearing in Table 1 were corrected on September 15, 2016. These guidelines were supported by a generous educational grant from Aratana Therapeu tics, Medtronic, and Zoetis. Every primary-care companion animal practice will encounter its Because oncology cases have the potential to create a strong share of oncology cases. This has never been truer since bond between the practice and the owner of a pet with cancer, improvements in pet nutrition, widespread heartworm control, primary-care veterinarians should be willing to consider treating renewed emphasis on age-specific preventive pet healthcare, regular select cases. The caveat in doing so is to ensure that the healthcare vaccinations, and senior pet screenings have led to a growing team is adequately trained and equipped to appropriately manage population of older dogs and cats. A section on safety discusses in detail the safety dogs), two-decade demographic study of the Veterinary Medical precautions and equipment that are appropriate when chemother Database found that neoplastic disease was the most common apeutic agents are used. These include the equipment needed and terminal pathological process in 73 of 82 canine breeds and the methods used to protect the clinic environment as well as the most common cause of death in dogs. Because oncology Each type of cancer and organ system involved has a particular cases are inevitable in clinical practice, some degree of expertise in progression to be considered when staging the case and presenting diagnosis and treatment of cancer is expected by clients and is an treatment options to the pet owner. A critical aspect of successful essential component of a comprehensive primary-care veterinary oncology case outcome is to develop a treatment plan specific for practice. Readers will find the two comprehen the purpose of these guidelines is to provide practice teams sive tables on common cancers of dogs and cats to be a concise and with guidance for accurate diagnosis and optimal management of useful resource for this purpose. Because almost all pet owners that the information in the tables should not be interpreted as a have some acquaintance with cancer in their own lives, they will ‘‘cookbook approach’’ to case management but rather a compila measure a veterinarian’s approach to managing an oncology case tion of relevant, tumor-specific information to help guide decision against their own experience. A sample case history is also provided so that practitioners other clinical situations, the client plays a prominent role in can consider how they would use the cancer tables to assess and directing how a pet’s cancer is managed. However, these guidelines do place Every cancer case is different, even if the type of neoplasia is special emphasis on three topics of paramount importance in commonplace. For this reason, these guidelines are specific in many oncology case management: safety in handling chemotherapeutic respects without being overly prescriptive. Within this framework, agents, delivery of radiation therapy, and relationships with the these guidelines offer the following sequential approach to owners of cancer patients. An personnel safety in handling chemotherapeutic agents, referral to underlying theme of these guidelines is that all staff members, an oncology specialty practice when appropriate, and a strong including clinical and administrative personnel, can positively emphasis on client support. A unified healthcare Because oncology patients are frequently of an advanced age, team that speaks with one voice will actively support a long-term their owners are often highly bonded to them and emotionally relationship with a client who entrusts the practice with the care of distraught after receiving a cancer diagnosis. When performing work together as a unified healthcare team and have a shared fine-needle sampling, aspiration is useful when the tissue is firm and understanding of the options, procedures, and expectations of may be of mesenchymal origin, but collecting samples without referral treatment. These include when the primary care training and experience, the general practitioner can often determine veterinarian or the client wishes to consider all possible treatment the presence and type of neoplasia in the office. Submission to a options or when the referring veterinarian cannot provide clinical pathologist for diagnostic confirmation is usually indicated optimum treatment for any reason. Cytology does not provide tumor grade information practices often have access to clinical trials in which the client may and may not always provide a clear-cut diagnostic result due to poor want to participate. Referrals are the goal of histopathology is to provide a definitive diagnosis appropriate when the primary care clinician can no longer meet the when unobtainable by cytology. Histopathology provides informa needs and expectations of the patient and client. The comfort level tion on tissue structure, architectural relationships, and tumor of the primary clinician and client with referral treatment will grade—results that are not possible with cytology. The tumor grade may guide the choice of treatment and provide importance of a clear, shared understanding of the referral process prognostic information. Proper technique is critical when perform by the pet owner, primary care veterinarian, and specific referral ing a surgical biopsy, particularly to obtain an adequate diagnostic specialists or referral centers cannot be overemphasized. It is also Obtain multiple samples from multiple locations within the important to recognize that a variety of specialists may be needed at tumor. After Biopsy deeply enough to penetrate any overlying normal or referral, it is important to establish a treatment plan for ongoing reactive tissue. Place samples in an adequate amount of formalin (10 parts formalin to 1 part tissue). Diagnosis of Tumor Type To avoid seeding adjacent normal tissue with cancer cells, Once the possibility of a neoplastic process is suspected, place the biopsy incision so that it can easily be excised at the determination of the tumor type serves as the basis for all time of definitive tumor removal. No confirmed diagnosis can be made by if (1) principles of appropriate surgical excision of tumors are palpation alone. A biopsy is the basic tool that allows removal and followed; and (2) staging procedures that might influence the examination of cells from the body to determine the presence, owner’s decision to have an excision performed have been cause, or extent of a disease process. Nodal metastasis seen more commonly and earlier than systemic (liver, bone, pelvis, lung). Often slowly progressive unless diffusely metastatic at diagnosis or compromised renal function due to hypercalcemia. Mast cell tumor Skin and subcutaneous Locally invasive; invasiveness increases with Pretreatment staging is optional for known tissues grade. Grade 1: metastases are rare Biopsy for determination of histologic grade is Grade 2:;20% advisable for any non-resectable, large or Grade 3:;100% rapidly growing tumor. Impact of local and nodal disease impacts quality of Primary radiation therapy (palliative or curative intent) life early in the disease process. A significant proportion of malignant tumors do not Lymph node metastases Consider complete mastectomy for dogs presenting metastasize and can be cured with appropriate High histologic grade with multiple tumors or developing multiple tumors surgery. When margins are histologically incomplete, local Mucous membrane locations Scar excision may be considered if margins are recurrence rates are ;20–30%. C-kit mutation be provided or margins are histologically Metastases Histologically incomplete surgical margins incomplete. Most patients with metastases eventually die Previous local recurrence Systemic treatment regardless of treatment. Survival periods are highly Systemic illness Vinblastine-based chemotherapy variable. Resection of ;1/3 lack melanin and may be confused with medial retro-pharyngeal, parotid and a sarcomas histologically. Liver A significant proportion Survival times are highly correlated with metastases cannot be definitively of splenic masses are clinical stage: distinguished from hyperplastic nodules. Optional definitively Stage 2: Hemoabdomen, no clinically Echocardiography for concurrent right atrial distinguished from detectable metastases.
Buy benadryl on line amex
The main ways used to try to stop cavernomas bleeding are neurosurgery and stereotactic radiotherapy allergy shots wiki order benadryl with a mastercard. In this operation, the skull is penetrated (called a ‘craniotomy’) and the cavernoma is removed. The method used and the risks involved depend on where the cavernoma is in the brain. Surgery for cavernomas has been made safer using the operating microscope (used in treatment called ‘microsurgery’). Brain scanning during the operation allows surgeons to reach cavernomas with as little disruption to the normal brain tissue as possible. This procedure is sometimes known as ‘image-guided surgical navigation’ or ‘computer-assisted or frameless stereotaxy’. Stereotactic radiotherapy involves beams of radiation being targeted at a brain cavernoma from many different points around the head. The radiotherapy beams are targeted very accurately, so it is important that the head does not move while a patient is being treated. Various techniques are used to keep the head still, such as the head frame shown in the picture. When radiotherapy is given as a one-off treatment, it is sometimes called ‘radiosurgery’. Unlike brain surgery, ‘radiosurgery’ does not involve a general anaesthetic or an operation. Stereotactic radiotherapy is usually carried out to treat cavernomas in regions where brain surgery would be too dangerous. It can be diffcult to decide whether or not to have treatment for a cavernoma that has caused symptoms. As mentioned above, these risks vary between patients in the short-term studies that have been done. The other thing to consider is the risk of treatment itself, which varies depending on where the cavernoma is and the type of treatment used. Before deciding whether to have treatment, you should talk to your doctor about your cavernoma. This can be useful when there is any uncertainty about the diagnosis of a cavernoma. However, even when diagnosis is certain, no features on a brain scan (such as signs that a cavernoma has grown) are known to show that the risk of bleeding would be higher. For most people, clear information from a doctor, and a clear discussion about whether or not to treat the cavernoma, is probably enough. As you can tell from reading this booklet, there are still many important questions about cavernomas which we do not yet have answers to . If you want more information about these, please read the ‘Genetics of brain cavernomas’ booklet. Such randomised controlled trials are the fairest test of whether treatment is benefcial. Along with our affliated organisation, Angioma Alliance, and associated groups throughout the world, we also provide updates on research. To make sure that every person with a brain cavernoma, and their family, has access to clear information about the illness. As you read this booklet, keep in mind that everyone recovers a little bit differently. A common cause of stress after a mild brain injury is worry about the symptoms you have. Scientific studies by neurosurgeons and neuropsychologists in New Zealand, Scandinavia, Great Britain, Can ada and the United States have shown that patients who get an information booklet like this one re cover faster and feel better during recovery than patients who do not know what to expect. You have been given this booklet so you will know what to expect and what to do about the symptoms you may experience. Your doctor can prescribe therapy and/ or medication that can help you if you need it. You can also talk to the person who gave you this booklet or call the number listed on the last page of this guide. This is because the brain is surrounded by shock-absorbing liquid and is covered by the skull, which usually is enough to protect the brain from any damage. When the skull fractures, it absorbs some of the force of the blow and protects the brain. This can sometimes cause the brain to get bruised if it hits the inside of the skull hard enough. If there are many bruises on the brain, there will be some swelling that can take a while longer to return to normal. Although these nerves cannot be seen without a microscope, we know that they can recover because many patients recover completely from mild brain injury in time. If there is bleeding deep inside the brain, then this is a sign of an injury that is more severe than a concussion. Bruises, swelling, snapped nerves and broken blood vessels are the causes of symptoms after a brain injury. Your doctors have examined you for any signs of injury to the brain and prescribed treatment if you need it. Most people who suffer a concussion recover completely in time because the damage is minor. Most doctors who treat people with brain injuries agree that recovery is faster when the patient gets enough rest and resumes responsibilities gradually. Some of these axons can snap or break during a concussion if it is serious enough. When this happens, different cells in your brain cannot com municate properly with each other. Even though we can only see axons under a microscope, we know that they can heal because in time many patients recover completely. Usu ally, the bleeding stops on its own and the blood vessels heal like any other cut does. Some of the “symptoms” you notice may have nothing to do with your concussion or injury. If you were not knocked out at all or were unconscious for less than 30 minutes, then the injury was most likely minor or mild. Although you may have some symptoms, there was probably little injury to the brain and complete recovery is expected. If the patient was knocked out for more than 30 minutes, but less than one hour, the injuries were most likely moderate. These symptoms are part of the normal recovery process and are not signs of permanent damage or medical complications. Like the itch of healing stitches, these symptoms are common and should not be a cause for concern or worry. A list of the symptoms that you can expect is shown below, along with the percent of mild brain injury patients who experience each symptom at some point in their recovery. The table also shows the percent of people who have these symptoms, even though no head injury occurred. When it becomes difficult to concentrate on what you are doing, take a break and relax for 15 to 30 minutes. Writing while you talk on the phone or taking notes as you listen to someone talk are examples of doing two things at the same time. You will probably be able to concentrate better when you have had enough rest or a short nap. Adjust your schedule and get more rest when you notice yourself becoming irritable. If you find yourself getting into arguments that cause trouble at home or at work, try to change the way you think about things. Problems can usually be solved better if you try to stay calm and explain your point of view.