Sarafem
Order sarafem 20 mg otc
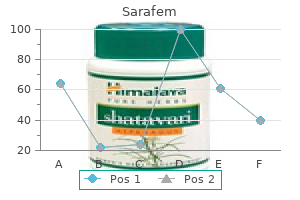
And the train came into the little station and it stopped and 5 people got onto the train and another person ran into the little station and got on women's health quick weight loss purchase sarafem in india, and 7 people got off the train and then the doors closed automatically and the train went away. And when the next train came I wasn’t so scared anymore because the sign said so I knew it was going to happen. And then I decided that I would look for Toby because there were only 3 people in the little station. So I stood up and I looked up and down the little station and in the doorways that went into tunnels but I couldn’t see him anywhere. And I walked after him and I bent down again and I said, “Toby Toby Toby,” and I held out my hand so that he could smell my hand and smell that it was me. And someone said, “Get out of there, for fuck’s sake,” and I looked up and it was a man who was wearing a green raincoat and he had black shoes and his socks were showing and they were gray with little diamond patterns on them. And the man with the diamond patterns on his socks tried to grab my shoulder, so I screamed. And then I heard the sound like sword fighting and Toby started running again, but this time he ran the other way, which was past my feet, and I grabbed at him and I caught him by the tail. And then the train came into the station and I stood up and I ran to the bench again and I put Toby into the pocket inside my jacket and he went very quiet and he didn’t move. And the man with the diamond patterns on his socks was standing next to me and he said, “What the fuck do you think you were playing at? And I said, “I’ve got a Swiss Army knife and it has a saw blade and it could cut someone’s fingers off. And the man with the diamond patterns on his socks said, “Mad as a fucking hatter. Jesus,” and he was pressing a handkerchief against his face and there was blood on the handkerchief. And then 8 more trains came and I decided that I would get onto a train and then I would work out what to do. And there were 11 people in the carriage and I didn’t like being in a room with 11 people in a tunnel, so I concentrated on things in the carriage. And there was a pattern on the walls which was like this: And there was a pattern on the seats like this: Then the train wobbled a lot and I had to hang on to a rail and we went into a tunnel and it was noisy and I closed my eyes and I could feel the blood pumping in the sides of my neck. And I timed the distance between stations all the way to Willesden Junction and all the times between stations were multiples of 15 seconds like this: 0:00 Paddington 1:30 Warwick Avenue 3:15 Maida Vale 5:00 Kilburn Park 7:00 Queen’s Park 10:30 Kensal Green 11:45 Willesden Junction And when the train stopped at Willesden Junction and the doors opened automatically I walked out of the train. And everyone who got off the train walked up a staircase and over a bridge except me, and then there were only 2 people that I could see and one was a man and he was drunk and he had brown stains on his coat and his shoes were not a pair and he was singing but I couldn’t hear what he was singing, and the other was an Indian man in a shop which was a little window in a wall. And I didn’t want to talk to either of them because I was tired and hungry and I had already talked to lots of strangers, which is dangerous, and the more you do something dangerous the more likely it is that something bad happens. And the map was covered with a grid and each square of the grid had two numbers on it. And I looked round Willesden Junction in a spiral, like when I was looking for the train station in Swindon, but on the map with my finger. And the man who had shoes that did not match stood in front of me and said, “Big cheese. And this was my route: So I went up the staircase and over the bridge and I put my ticket in the little gray gate and went into the street and there was a bus and a big machine with a sign on it which said English Welsh and Scottish Railways, but it was yellow, and I looked around and it was dark and there were lots of bright lights and I hadn’t been outside for a long time and it made me feel sick. So I started walking, but Siobhan said I didn’t have to describe everything that happens, I just have to describe the things that were interesting. So I decided to wait and I hoped that Mother was not on holiday because that would mean she could be away for more than a whole week, but I tried not to think about this because I couldn’t go back to Swindon. And a lady came into the garden and she was carrying a little box with a metal grille on one end and a handle on the top like you use to take a cat to the vet, but I couldn’t see if there was a cat in it, and she had shoes with high heels and she didn’t see me. And then it started to rain and I got wet and I started shivering because I was cold. And a voice said, “I don’t care whether you thought it was funny or not,” and it was a lady’s voice. And the other voice, which was the lady’s voice, said, “Well, perhaps you should have thought about that before you made me look like a complete idiot. And I took Father’s cashpoint card so I could get money out and a policeman helped me. Shears said, “Are you going to come in or are you going to stay out here all night? Shears up the stairs and there was a landing and a door which said Flat C and I was scared of going inside because I didn’t know what was inside. And Mother said, “Go on or you’ll catch your death,” but I didn’t know what you’ll catch your death meant, and I went inside. And then she said, “I’ll run you a bath,” and I walked round the flat to make a map of it in my head so I felt safer, and the flat was like this: And then Mother made me take my clothes off and get into the bath and she said I could use her towel, which was purple with green flowers on the end. I kept thinking something dreadful had happened, or you’d moved away and I’d never find out where you were. And then you had a heart attack and died and he kept all the letters in a shirt box in the cupboard in his bedroom and I found them because I was looking for a book I was writing about Wellington being killed and he’d taken it away from me and hidden it in the shirt box. And then she made a loud wailing noise like an animal on a nature program on television. And I didn’t like her doing this because it was a loud noise, and I said, “Why are you doing that? But I didn’t have any pajamas so I put on a white T-shirt and a pair of yellow shorts which were Mother’s, but I didn’t mind because I was so tired. And then I heard someone opening the door of the flat and there was a strange man’s voice outside, so I locked the bathroom door. And there was an argument outside and a man said, “I need to speak to him,” and Mother said, “He’s been through enough today already,” and the man said, “I know. And there was a policeman outside the door and he said, “Are you Christopher Boone? And the policeman said, “If your husband turns up and causes any trouble, just give us a ring. Shears stacked up some boxes in the spare room so he could put a blowup mattress on the floor for me to sleep on, and I went to sleep. And then I woke up because there were people shouting in the flat and it was 2:31 a. And then Mother said, “I think you should go now,” but she was talking to Father, not me. Shears had rung the police station and he told Father to calm down and he took him out of the flat. And people catch it because of the meaning of something an infected person says and the meaning of what they do with their faces when they say it, which means that people can also get it from watching an infected person on television, which means that it spreads around the world really quickly. And when people get the virus they just sit on the sofa and do nothing and they don’t eat or drink and so they die. But sometimes I have different versions of the dream, like when you can see two versions of a film, the ordinary one and the director’s cut, like Blade Runner. And in some versions of the dream the virus makes them crash their cars or walk into the sea and drown, or jump into rivers, and I think that this version is better because then there aren’t bodies of dead people everywhere. And eventually there is no one left in the world except people who don’t look at other people’s faces and who don’t know what these pictures mean and these people are all special people like me. And they like being on their own and I hardly ever see them because they are like okapi in the jungle in the Congo, which are a kind of antelope and very shy and rare. But if I don’t want to go anywhere I don’t have to , and I can stay at home and eat broccoli and oranges and licorice laces all the time, or I can play computer games for a whole week, or I can just sit in the corner of the room and rub a £1 coin back and forward over the ripple shapes on the surface of the radiator. And I go out of Father’s house and I walk down the street, and it is very quiet even though it is the middle of the day and I can’t hear any noise except birds singing and wind and sometimes buildings falling down in the distance, and if I stand very close to traffic lights I can hear a little click as the colors change. And I go into other people’s houses and play at being a detective and I can break the windows to get in because the people are dead and it doesn’t matter. And I take a ladder from Father’s van and I climb up onto the roof, and when I get to the edge of the roof I put the ladder across the gap and I climb to the next roof, because in a dream you are allowed to do anything. And then I find someone’s car keys and I get into their car and I drive, and it doesn’t matter if I bump into things and I drive to the sea, and I park the car and I get out and there is rain pouring down. And I go home to Father’s house, except it’s not Father’s house anymore, it’s mine. The next morning I had fried tomatoes for breakfast and a tin of green beans which Mother heated up in a saucepan. Shears had gone to work she made a telephone call to the office and took what is called Compassionate Leave, which is when someone in your family dies or is ill. So we went out of the flat and we walked to the main road, which was Hill Lane, which was the A4088, and it was really crowded and we caught a number 266 bus to Brent Cross Shopping Centre.
Order discount sarafem on-line
Laboratory services Medicare covers laboratory services including certain blood tests women's health center murfreesboro tn purchase sarafem 20mg, urinalysis, certain tests on tissue specimens, and some screening tests. You generally pay nothing for this service if the health care provider accepts assignment. Note: Before your frst lung cancer screening, you’ll need to schedule an appointment with your doctor to discuss the benefts and risks of lung cancer screening. You pay nothing for these preventive services because the deductible and coinsurance don’t apply. Coverage includes services generally provided in an outpatient setting (like a doctor’s or other health care provider’s office, or hospital outpatient department), including visits with a psychiatrist or other doctor, clinical psychologist, nurse practitioner, physician assistant, clinical nurse specialist, or clinical social worker. Generally, you pay 20% of the Medicare-approved amount and the Part B deductible applies for mental health care services. This counseling is covered if you get it in a primary care setting (like a doctor’s office), where it can be coordinated with your other care and a personalized prevention plan. You pay nothing for this service if the doctor or other qualified health care provider accepts assignment. Occupational therapy Medicare covers evaluation and treatment to help you perform activities of daily living (like dressing or bathing) to maintain current capabilities or slow decline when your doctor or other health care provider certifies you need it. Opioid use disorder treatment services Starting January 1, 2020, Medicare will cover opioid use disorder treatment services provided by opioid treatment programs. The services will include medication, counseling, drug testing, and individual and group therapy. Counseling and therapy services will be covered in person and by virtual delivery (using 2-way audio/video communication technology). Under Original Medicare, you will pay nothing for these services if you get them from an opioid treatment provider who’s enrolled in Medicare. Talk to your doctor or other health care provider to find out where you can go for these services. Generally, you pay 20% of the Medicare-approved amount for the doctor’s or other health care provider’s services. You may pay more for services you get in a hospital outpatient setting than you’ll pay for the same care in a doctor’s office. In addition to the amount you pay the doctor, you’ll also usually pay the hospital a copayment for each service you get in a hospital outpatient setting, except for certain preventive services that don’t have a copayment. In most cases, the copayment can’t be more than the Part A hospital stay deductible for each service. If you get hospital outpatient services in a critical access hospital, your copayment may be higher and may exceed the Part A hospital stay deductible. Get estimated costs of outpatient procedures performed in hospital outpatient departments by visiting Medicare. Outpatient medical and surgical services and supplies Medicare covers approved procedures like X-rays, casts, stitches, or outpatient surgeries. You pay 20% of the Medicare-approved amount for the doctor’s or other health care provider’s services. You generally pay the hospital a copayment for each service you get in a hospital outpatient setting. In most cases, for each service provided, the copayment can’t be more than the Part A hospital stay deductible. The Part B deductible applies, and you pay all costs for items or services that Medicare doesn’t cover. Physical therapy Medicare covers evaluation and treatment for injuries and diseases that change your ability to function, or to maintain current function or slow decline, when your doctor or other health care provider certifies your need for it. Pneumococcal shots Medicare covers pneumococcal shots (or vaccines) to help prevent pneumococcal infections (like certain types of pneumonia). Medicare covers the first shot at any time, and also covers a different second shot if it’s given one year (or later) after the first shot. Talk with your doctor or other health care provider to see if you need one or both of the pneumococcal shots. You pay nothing for these shots if the doctor or other qualified health care provider accepts assignment for giving the shots. You pay 20% of the Medicare-approved amount for these covered drugs, and the Part B deductible applies. If the covered drugs you get in a hospital outpatient setting are part of your outpatient services, you pay a copayment for the services. However, other types of drugs in a hospital outpatient setting (sometimes called “self-administered drugs” or drugs you’d normally take on your own) aren’t covered by Part B. What you pay depends on whether you have Part D or other prescription drug coverage, whether your drug plan covers the drug, and whether the hospital’s pharmacy is in your drug plan’s network. Contact your prescription drug plan to find out what you pay for drugs you get in a hospital outpatient setting that aren’t covered under Part B. Other than the examples above, you pay 100% for most prescription drugs, unless you have Part D or other drug coverage. For the digital rectal exam, you pay 20% of the Medicare-approved amount, and the Part B deductible applies. Prosthetic/orthotic items Medicare covers arm, leg, back, and neck braces; artificial eyes; artificial limbs (and their replacement parts); and prosthetic devices needed to replace an internal body organ or function of the organ (including ostomy supplies, parenteral and enteral nutrition therapy, and some types of breast prostheses after a mastectomy) when ordered by a doctor or other health care provider enrolled in Medicare. For Medicare to cover your prosthetic or orthotic, you must go to a supplier that’s enrolled in Medicare. You pay 20% of the Medicare-approved amount if you get the service in a doctor’s office. You also pay the hospital a copayment per session if you get the service in a hospital outpatient setting. Generally, you’re responsible for paying 20% of the charges, and the Part B deductible applies. Second surgical opinions Medicare covers second surgical opinions for surgery that isn’t an emergency. Medicare covers these tests once every 12 months or at certain times during pregnancy. Medicare will only cover these counseling sessions if they’re provided by a primary care doctor or other primary care provider and take place in a primary care setting (like a doctor’s office). Counseling conducted in an inpatient setting, like a skilled nursing facility, won’t be covered as a preventive service. You pay nothing for these services if the primary care doctor or other qualified health care provider accepts assignment. You pay nothing for the counseling sessions if the doctor or other qualified health care provider accepts assignment. Speech-language pathology services Medicare covers evaluation and treatment to regain and strengthen speech and language skills, including cognitive and swallowing skills, or to maintain current function or slow decline, when your doctor or other health care provider certifies you need it. Surgical dressing services Medicare covers medically necessary treatment of a surgical or surgically treated wound. You pay a fixed copayment for these services when you get them in a hospital outpatient setting. Telehealth Medicare covers services like office visits, psychotherapy, consultations, and certain other medical or health services provided by an eligible provider who isn’t at your location using an interactive, two-way telecommunications system (like real-time audio and video). These services are available in rural areas, under certain conditions, but only if you’re located at: a doctor’s office, hospital, critical access hospital, Rural Health Clinic, Federally Qualified Health Center, hospital-based dialysis facility, skilled nursing facility, or community mental health center. For most of these services, you’ll pay the same amount that you would if you got the services in person. Starting in 2020, Medicare Advantage Plans may ofer more telehealth benefts than Original Medicare. These benefts will be available no matter where you’re located, and you can use them at home instead of going to a health care facility. If you get the test at a hospital as an outpatient, you also pay the hospital a copayment that may be more than 20% of the Medicare-approved amount, but, in most cases, this amount can’t be more than the Part A hospital stay deductible. Transitional care management services Medicare may cover this service if you’re returning to your community after a stay at certain facilities, like a hospital or skilled nursing facility. The health care provider who’s managing your transition back into the community will work to coordinate and manage your care for the frst 30 days after you return home. He or she will work with you, your family, and caregiver(s), as appropriate, and other health care providers. You’ll also be able to get an in-person ofce visit within 2 weeks of your return home. The health care provider may also review information on the care you received in the facility, provide information to help you transition back to living at home, work with other care providers, help you with referrals or arrangements for follow up care or community resources, assist you with scheduling, and help you manage your medications.
Purchase generic sarafem pills
Together with her husband menstrual quotes order generic sarafem canada, she farms a small lot and maintains a home with their children. To make up for the lack of breastmilk during the day, she chews pieces of meat and mixes them with the rice por ?My day starts very early, because of the long walk to the ridge that she has prepared for Kaka in the morning. Because of this, her breastfeeding prac heavy workload means Xaiathon is also unable to follow tice is not as regular as her doctor has advised. For example, many cultures the rise in the promotion, sales and use believe babies should not consume of breastmilk substitutes, including follow colostrum and should be fed another liquid, on formulas and toddler milks, is an area such as sugar water, honey or animal of growing concern. Global sales grew by 53 cent in Latin America and Caribbean, per cent between 2008 and 2013. When these mothers take raised concerns about the rise in antiretroviral medicine consistently the use of toddler milks. What are young children eating Except for breastmilk, based on country the percentage of young income level? The percentage of children consuming non-dairy animal source foods such as eggs, meat, poultry and fsh in upper-middle income countries is nearly twice as high as those in low and lower-middle-income countries. Estimates by World Bank income groups are only displayed if available data represents at least 50 percent of the population. Nearly half of children 4?5 frequently cited barrier to exclusive months of age and around 15 per breastfeeding. Fish and development and preventing which is relatively cheap and protein overweight/obesity later in life. Previously, parents in cluding community radio stations, Rwanda begin to slide into the dri this community would have thought community health workers (who er, fatter savannahs. Twenty-two it natural to feed young children a hold monthly growth-monitoring children in her village used to suffer diet heavy in carbohydrates such sessions and cooking demon from undernutrition, but today, not as potatoes. Now they know this is strations), agricultural technicians a single child is considered either not enough: diverse fruits, legumes, (who teach communities to create severely or moderately undernour grains, vegetables, and sources of kitchen gardens), and members of ished. Much of this improvement protein such as eggs, fsh, meat and village savings and loans groups. Denise and her fellow community health workers across Rwanda are ?At frst, people did not think about Through cooking sessions in her in the vanguard of the fght against feeding children vegetables and home, Denise demonstrates tech undernutrition, for which prompting other healthy foods, Denise says. As long as we keep informing and ers how to make beet juice, which is resources, the government rolled encouraging people, no more chil rich in vitamins and minerals. Fortifed complementary foods or multiple As any parent knows, infants and toddlers micronutrient powders can help close can be fussy eaters. Around the world, a preferences can change from week to range of fortifed blended foods high week and parents often offer what the in proteins and micronutrients are child prefers. As of 2017, programmes crisps, and cakes was that ?the child providing micronutrient powders likes it, far outweighing other factors had been implemented in at least 47 such as affordability, convenience or countries, reaching over 16 million perceptions that the foods were healthy. Infants the study found that, in all four cities, and young children also beneft from young children were more likely to eat eating large-scale, centrally processed commercially produced snack foods than fortifed foods such as iodized salt, foods rich in micronutrients, such as leafy iron-fortifed fours and vitamin-A green and orange-feshed vegetables. For example, in Nairobi, Children who are Kenya, such products meet around a At the same time, a growing body of hungry at school quarter of the vitamin A requirement evidence from high-income countries struggle to pay and half the iron requirement of children indicates that commercial foods available attention and between 6 and 23 months of age. Thanks to a set of cards self-esteem and social status within breastfeed her 3-month-old baby with simple drawings, she and 29 their communities. Women were so James exclusively until he is 6 months other women were taught how to proud of their achievements that they old and then to give complementary help prevent their children catching organized a graduation ceremony at food in addition to breastmilk to keep diseases or suffering from malnu their own expense. They learned that breastmilk atrice Rubin of the Paillant health cen was not exclusively breastfed. After contains all the nutrients required by tre, vaccine coverage is nearly 100% three months, I gave him water and babies and no other food or liquid is for ante and post-natal consultations food almost every day. Referrals of malnourished chil nutrient-dense meals of purees using dren are more numerous since the the 25-year-old mother, who sold sec local ingredients. Only 40% of soup, with corn and dry fsh, to feed my child well-being and development. The mum acceptable feeding practices, al knowledge from the local Paillant club is participative, interactive and and more than 1 in 5 children aged Mothers Club in her town of Les joyful. With three quarters into toddlerhood, early introduction, products with high of all newborns delivered with the they start to choose amounts of sugar, use of artifcial help of a skilled birth attendant, these their own food and favours, inappropriate consistency providers have a signifcant impact on are exposed to new for developing eating behaviours, and breastfeeding uptake and practices. However, their advice can often be opening them to new infuences aside inappropriate insisting, for example, from their parents and caregivers. At that colostrum is ?dirty and urging this age, positive models of eating mothers to hold off feeding animal from parents, caregivers, siblings, source foods until the child is 18 months educators and peers become more of age. It can development in environments where undernutrition refect situations where the caregiver takes control and is prevalent. The retail sector determines the growth spurts and decrease during availability of and access to breastmilk slower growth periods. One study supermarkets can make it diffcult for conducted in 2010 in Peru found that parents and children to make healthy stunted children who caught up by the food choices. Low Middle childhood: A time of consumption of fruits and vegetables transition (ages 5?9) is common a worrying phenomenon given that children who eat fruits and vegetables in childhood are more likely When children start going to primary to continue doing so into adulthood. This period of transition for example, no children aged 7?8 years is important for establishing healthy met the diet quality index for vegetables. At this age, traditional Children in developing countries, gender roles and expectations begin especially in poorer households and to take hold for many children in low rural areas, tend to have diets made and middle-income settings, with girls up of a few staples such as cereals, often helping out in the kitchen and roots or tubers with little protein. How diet, cognitive development and much children eat during this phase academic achievement. Energy these challenges, several initiatives have obesity in middle is essential for concentration and been launched. Rice, the Bhutanese childhood has participation in school activities, staple food, has been fortifed and is both short and so children who have an empty now supplied to all schools. School long-term effects stomach and feel hungry at school menus are also reviewed to increase from skipping breakfast or not diversity and nutrition in meals. School-age nutritional risks and concerns Hidden hunger also impairs school performance; certain micronutrient Overweight (and obesity) in middle defciencies affect learning. According childhood has both short and long to research, iron defciency is linked term effects. Research has found that children Micronutrient defciencies are a major in sub-Saharan Africa, especially in challenge one in three adolescent girls urban areas and among higher-income in Bhutan is anaemic, and iron defciency households, are sitting more and is thought to be a major cause. In 2017, exercising less, which has implications a government analysis revealed that for their health and nutrition. In 2010, the government established food and beverage It may seem counter-intuitive, but in guidelines for elementary schools. According to foods prohibited in the guidelines research conducted in New Zealand were still widely available, while in 2007, this is because children who vegetables, fruits, and plain water miss or skip breakfast subsequently eat accounted for less than 7 per cent more snacks cookies, sweets, chips of the foods and drinks available in or crisps, and sweetened carbonated schools. In vulnerable to rural areas, they often have limited food (ages 10?19) undernutrition, options and are susceptible to seasonal in part because food shortages. In urban areas, they are their rapid physical Adolescence is a time of rapid physical surrounded by fast food and nutrient growth and and psychosocial development and poor snacks and drinks. Half of adolescent girls in low will be 250 million more adolescents income and rural settings in low and compared with just 30 years ago. Proper middle-income countries eat fewer than Padma, 17, chats with members of nutrition for this large cohort is important three meals a day, with most missing or the Adolescent Girls Club at Muttock Tea Estate, Dibrughar district, Assam, for both their current and future well skipping breakfast. Yet around the world, adolescents during school hours, and lunch is usually about the risks of drinking salt tea. When fast foods were considered as intake meals purchased outside the home, 93% of adolescent girls from low and middle-income countries globally were found to consume Adolescents Adolescents from More adolescents More adolescents them at least weekly. Undernutrition in adolescence is associated Adolescents are especially vulnerable with impaired cognitive function, school to undernutrition, in part because their absenteeism and psychological stress. The absence of adequate nutrition on Nutrition and chief of adolescent medicine risks undermining this crucial period of at Stanford University School of Medicine growth and development, an impact that in California, has said, ?If [teens] don?t eat is compounded for the 16 million girls right, they can become irritable, depressed between 15 and 19 years old and the 2. There is some for high return individuals who drank sugar water evidence that obesity in adolescence on investment during adolescence showed less can have lifelong negative effects on with nutritional motivation and pursued rewards the brain, contributing to early onset of interventions as adults, behaviours that signify cognitive dysfunction during ageing. To support their rapid growth around 16 million adolescent girls and physical development, adolescents aged 15?19 give birth.
Sarafem 20mg without prescription
Unless a baseline is established when the person is healthy pregnancy 8 weeks 10mg sarafem visa, it is difficult to know whether there has been a deterioration later in life. By the time an individual is referred with concerns, considerable deterioration may have already occurred and an accurate account of pre-morbid functioning may be difficult to construct. Longitudinal data is then needed to establish decline from a baseline as it is not possible to compare results of an assessment with an ‘average’ result for the person with Down’s syndrome, intellectual disabilities or general population. Whilst it may be possible to establish a diagnosis of dementia from a one-off assessment when there is good historic data from which to compare, or the clinical picture is extremely clear, there is a risk of false negative or positive diagnoses. Prompt diagnosis ensures that attention can be paid in a timely way to necessary changes to a care package, medication, preparing family carers and support staff for the inevitable changes and challenges that dementia will bring. There is currently no clear evidence base as to the best age at which this should occur; however, setting a baseline when the client is healthy and functioning at their best will clearly be most helpful at re-screen should concerns arise. It has been suggested that an assessment by the age of 30 years would be helpful (Turk et al. Ongoing neurodevelopment in late adolescence and early adulthood should be considered so as not to set baselines at too early an age when the brain is still developing. Carr (2000) demonstrated stability in intellectual ability and daily living skills for her cohort of people with Down’s syndrome during the age period 21–30 years. This suggests that a baseline conducted by the age of 30 would helpfully capture people prior to any cognitive decline. Ideally, a baseline assessment at age 30 years would capture an individual’s functioning once the brain is thought to be relatively fully developed, and before the potential onset of 14 Dementia and People with Intellectual Disabilities dementia. A copy of the baseline assessment should be given to the person and their carers to keep in the person’s health action plan for future reference. Functional limitations of electronic health record systems may require the development of additional databases to capture relevant clinical information about clients with Down’s syndrome, or people on dementia care pathways. It is important to be aware of relevant data protection issues and organisational protocols (such as registering your database with the Trust’s information governance department) and be mindful of the potential need to gain consent/assent from service users and/or their carers to have personal information recorded in such a way. Some services seek simultaneous consent for inclusion on dementia databases alongside permissions to contact clients regarding possible research projects that may be of interest in the future. This necessitates, as do baseline assessments, having a register of all adults with Down’s syndrome and additionally a method of recalling people for a re-assessment. The frequency of prospective monitoring for dementia should be matched to the rising risk with age. For example, the baseline assessment should take place at 30 years; then every two years for those in their 40s; and annually for those aged 50 and over. Assessment is non-invasive and is usually enjoyable for the participant (see Section 6). Additional benefits of regular assessment One argument in favour of prospective screening concerns the known health risks for all people with Down’s syndrome. Many treatable illnesses can produce symptoms of cognitive decline independent of dementia. The evidence is that all too often, such disorders remain undetected in intellectual disabilities populations (Watchman, 2014). This applies particularly to people with Down’s syndrome who are prone to certain health problems (Coppus, 2014). There are useful factsheets, available free of charge on the internet from the Down’s Syndrome Association, that can be used to raise awareness of this issue. A review of six months of routine prospective screens carried out in one intellectual disability service showed that of 33 prospective assessments of apparently healthy adults with Down’s syndrome, 12 (36 per cent) revealed concerns that had not previously been identified by carers. These included dementia-like symptoms (memory and behavioural change), physical or mental health concerns that could be immediately treated, and action required by social services, including one requiring the instigation of the safeguarding protocol (Major & McBrien, 2011). Guidance on their Assessment, Diagnosis, Interventions and Support 15 Prospective assessments – should we or shouldn’t we? The evidence does not currently indicate a need for prospective screening for people with intellectual disabilities without Down’s syndrome. Screening for people with Down’s syndrome needs to be justified in terms of likely gain, the demands placed on the service, and there needs to be consideration of the issue of informed consent. Some services may decide against it for reasons of intrusion, commissioning intentions and/or resource limitations. Apparent changes in scores on cognitive assessments do not in themselves indicate dementia but do require further investigation. This will enable the progression of the disease to be described, suitable medical, psychosocial and environmental interventions to be put in place, and the quality outcome for the person to be measured. Key points I It is recommended to assess every adult with Down’s syndrome by the age of 30 to establish a baseline against which to compare future suspected changes in functioning. I It is worth considering screening all adults with Down’s syndrome over 40 regularly because of the increased risk of dementia and the prevalence of undetected but treatable illnesses. I Once the person has been suspected of having dementia, a programme of regular monitoring and reassessment needs to be established. It is important to remember, however, that some changes may be part of the normal ageing process. There are a number of other reasons an individual with intellectual disabilities may show a cognitive decline. The list below, whilst not exhaustive, describes the most common reasons for change in ability. Dementia: the typical presentation of dementia is one of gradual loss of skills along with change in personality and cognitive decline. Dementia is a diagnosis of exclusion therefore, it is important to consider other conditions that may cause loss of skills and cognitive decline, especially as many of these are treatable. Physical problems include such conditions as hypothyroidism, anaemia, uncontrolled epilepsy and chronic infections. Electrolyte abnormalities, hypo or hyper-glycaemia, nutritional deficiencies particularly vitamin B12 or folate could also cause functional decline in adults with intellectual disabilities. A thorough physical examination and relevant clinical tests are required at the time of initial assessment. Sensory impairments: People with intellectual disabilities in general and those with Down’s syndrome in their middle/old age specifically are likely to develop hearing and visual impairments. Visual impairment could be due to development of cataract or conditions such as keratoconus in individuals with Down’s syndrome. Some 60–80 per cent of people with Down’s syndrome will have hearing problems at some point in their lives. Conductive hearing deficit caused by earwax and the narrow acoustic canal is frequently seen in people with Down’s syndrome. Mental health problems: the most common differential diagnosis is depressive illness (McBrien, 2003) but other conditions such as the exacerbation of an existing psychotic disorder can mimic the presentation of dementia. Sleep problems: Obstructive sleep apnoea or other sleep disorders can cause day time drowsiness, mental slowing as well as confusion, and are particularly common in people with Down’s syndrome. Day time drowsiness and slowing could be interpreted as dementia if the sleep problem is not identified. Iatrogenic (medication related) causes: Medications with anticholinergic side effects can cause cognitive impairments in elderly people and people with intellectual disabilities. Use of high dose psychotropic/anti-epileptic medications and multiple medications can contribute to cognitive impairment as well. Some of the common medications that could cause a dementia-like presentation are listed in Table 1. Guidance on their Assessment, Diagnosis, Interventions and Support 17 Table 1: Some common medications that could cause a dementia-like presentation (Diagnosis and treatment guideline, Mayo Foundation for Medical Education and Research, (Moran et al. Impact of life events: People with intellectual disabilities in their middle age can face a number of life events such as loss of a parent or long-term carer, moving away from home or loss of day activities. In some individuals, the impact of life events may lead to a regressive state with apparent loss of skills. Changes in routine such as new structure to day opportunities or changes in support staff can cause profound reactions in an individual with intellectual disabilities leading to functional decline and a dementia like presentation. Abuse: Current or recent physical, emotional or sexual abuse in people with intellectual disabilities may result in loss of skills and regression and the development or exacerbation of behaviour problems that might superficially mimic dementia. Impact of poor environment: An unsuitable environment associated with a lack of stimulation, isolation and lack of social opportunities for positive interaction can lead to loss of skills. In the event that this is also associated with changes in support structure, where people do not know the individual well, these changes may be attributed to dementia.
Order online sarafem
This guideline focuses on: (1) Practice recommendations: directed at the nurse to guide practice regarding assessment and screening for delirium menstruation education generic 20 mg sarafem with amex, dementia and depression in older adults; (2) Education recommendations: directed at educational institutions and organizations in which nurses work to support its implementation; (3) Organization and policy recommendations: directed at practice settings and the environment to facilitate nurses’ practice; (4) Evaluation and monitoring indicators. Although this guideline is written to guide nursing practice, geriatric mental healthcare is an interdisciplinary endeavour. Many settings have formalized interdisciplinary teams and the panel strongly supports this structure. Collaborative assessment and treatment planning with the client and family are essential. It is acknowledged that the screening for delirium, dementia and depression needs to be studied in a more clearly defined way, and that there are gaps in the research evidence. However, this guideline will enable nurses to apply the best available evidence to clinical practice, and to promote the most appropriate use of healthcare resources. Screening for Delirium, Dementia and Depression in Older Adults All nurses are in a position to flag changes in a client’s mental health status and direct the client to appropriate care. It is expected that individual nurses will perform only those aspects of geriatric mental health assessment and intervention/management within their scope of practice. At the onset the panel discussed and came to a consensus on the scope of the best practice guideline. A search of the literature for systematic reviews, clinical practice guidelines, relevant articles and websites was conducted. The panel identified a total of twenty clinical practice guidelines related to geriatric mental health assessment and management. An initial screening was conducted with the following inclusion criteria: Guideline was in English, international in scope. Ten guidelines were short-listed for critical appraisal using the “Appraisal Instrument for Clinical Practice Guidelines” (Cluzeau et al. This tool allowed for the evaluation in three key dimensions: rigour, content and context and application. Recognition and initial assessment 17 of Alzheimer’s disease and related dementias. Department of Health and Human Services, Public Health Service, Agency for Healthcare Policy and Research. Iowa City: the University of Iowa Gerontological Nursing Interventions Research Center, Research Development and Dissemination Core. Through a process of evidence gathering, synthesis and consensus, a draft set of recommendations was established. This draft document was submitted to a set of external stakeholders for review and feedback – an acknowledgment of these reviewers is provided at the front of this document. Stakeholders represented various healthcare professional groups, clients and families, as well as professional associations. The results were compiled and reviewed by the development panel – discussion and consensus resulted in revisions to the draft document prior to pilot testing. Practice settings in Ontario were asked to submit a proposal if they were interested in pilot testing the recommendations of the guideline. These proposals were then subjected to a review process, from which a successful practice setting was identified. A nine-month pilot implementation was undertaken to test and evaluate the recommendations in three hospitals in Toronto, Ontario. An acknowledgment of these organizations is included at the front of this document. The development panel reconvened after the pilot implementation in order to review the experiences of the pilot sites, consider the evaluation results and review any new literature published since the initial development phase. All these sources of information were used to update/revise the document prior to publication. Clinical Practice Guidelines or Best Practice Guidelines: Systematically developed statements (based on best available evidence) to assist practitioner and client decisions about appropriate healthcare for specific clinical (practice) circumstances (Field & Lohr, 1990). Consensus: A process for making policy decisions, not a scientific method for creating new knowledge. At its best, consensus development merely makes the best use of available information, be that of scientific data or the collective wisdom of the participants (Black et al. Education Recommendations: Statements of educational requirements and educational approaches/strategies for the introduction, implementation and sustainability of the best practice guideline. Evidence: “An observation, fact or organized body of information offered to support or justify inferences or beliefs in the demonstration of some proposition or matter at issue” (Madjar & Walton, 2001, p. Nursing Best Practice Guideline Meta-Analysis: the use of statistical methods to summarize the results of independent studies, thus providing more precise estimates of the effects of healthcare than those derived from the individual studies included in a review (Clarke & Oxman, 1999). Organization & Policy Recommendations: Statements of conditions required for a practice setting that enable the successful implementation of the best practice guideline. Practice Recommendations: Statements of best practice directed at the practice of healthcare professionals that are ideally evidence-based. Stakeholder: A stakeholder is an individual, group or organization with a vested interest in the decisions and actions of organizations who may attempt to influence decisions and actions (Baker et al. Stakeholders can be of various types, and can be divided into opponents, supporters, and neutrals (Ontario Public Health Association, 1996). Systematic Review: Application of a rigorous scientific approach to the preparation of a review article (National Health and Medical Research Council, 1998). Systematic reviews establish where the effects of healthcare are consistent and research results can be applied across populations, settings, and differences in treatment. The use of explicit, systematic methods in reviews limits bias (systematic errors) and reduces chance effects, thus providing more reliable results upon which to draw conclusions and make decisions (Clarke & Oxman, 1999). Screening for Delirium, Dementia and Depression in Older Adults Background Context Prevalence studies indicate that the size of the older adult population is increasing and is projected to continue to increase. The Canadian Study on Health and Aging Working Group (1994b) estimated that in 1991, 12 percent of the population was over the age of sixty-five years and reported that this figure will rise to 21. Delirium, dementia and depression are often unrecognized among the geriatric population, due to their complexity and multi-faceted nature. This lack of recognition impacts on the quality of life, morbidity and mortality of the older client. Enabling the nurse to recognize and provide timely screening for delirium, dementia and depression may result in improved 20 outcomes for the client. Delirium is a temporary disordered mental state, characterized by acute and sudden onset of cognitive impairment, disorientation, disturbances in attention, decline in level of consciousness or perceptual disturbance. A prevalent disorder, it is estimated that 14 to 80 percent of all elderly clients hospitalized for the treatment of acute physical illnesses experience an episode of delirium. Studies have shown a marked variability in the epidemiology of delirium results from the differences in study populations, diagnostic criteria, case finding and research techniques (Foreman, Wakefield, Culp & Milisen, 2001). Research findings have shown that delirium in older adults result in: greater in-hospital functional decline (Foreman et al. Nursing Best Practice Guideline Dementia is a syndrome of progressive decline in multiple areas of cognitive function eventually leading to a significant inability to maintain occupational and social performance. Research shows there are presently over 250,000 seniors with dementia in Canada, and it is estimated to rise to 778,000 by 2031 (Canadian Study on Health and Aging, 1994b; Patterson et al. The incidence suggests that there will be approximately 60,150 new cases of dementia in Canada each year. Depressive symptoms occur in 15 to 20 percent of community-based elders requiring clinical attention and 37 percent of elders in primary care settings. Mortality and morbidity rates increase in the older adult experiencing depression, and there is a high incidence of comorbidity with medical conditions (Conwell, 1994). It is widely known that depression can lead to increased mortality from other diseases such as heart disease, myocardial infarction, cancer and chronic depression (U. Untreated depression may also result in increased substance abuse, slowed recovery from medical illness or surgery, malnutrition and social isolation (Katz, 1996). The most troubling outcome of depression is elder suicide, and older adults have the highest risk of suicide rates of any age group. The suicide rate for individuals aged 85 and older is the highest at about 21 suicides per 100,000 people, a 25 percent increase from 1980 to 1986 (Conwell, 1994). Studies reveal that single, white, elderly males have the highest rate of suicide and are more likely to succeed than their female counterparts.
Cheap sarafem 20 mg fast delivery
The hallucinations were not significantly related to the severity of dementia womens health 5k training cheap sarafem 20mg with mastercard, although subjects with very mild dementia did not experience auditory hallucinations. A study by Mendez suggested that person misiden tification in dementia begins with an altered sense of familiarity for a familiar person [287]. Johansson and Gustafson followed a sample of dementia patients treated at a psycho geriatric day hospital by means of a standardized clinical evaluation during an average of 21 14 months [292]. The clinical features were related to clinical diagnoses, and their first appearance was early, late or intermittently during the course of dementia. This high prevalence was probably due to close communication between the patient and the contact person, allowing for early recognition of clinical changes and the appearance of new symptoms, even those of short duration. Delusions were significantly associated with physical aggression but accounted for only 3. An interesting finding was that episodes of physical aggression occurred during interactions of caregivers with the patient and that verbal aggression occurred in situations where the patient was being instructed by the caregiver. The study showed an association with functional impairment, although deluded patients showed better attention than non-deluded patients. The delusions were most often described as simple, non-systematic and unelaborated. Moreover, visual hal lucinations are significantly associated with impaired visual acuity and cognitive impairment [297]. Delusions, especially paranoid, in dementia are inversely related to cortical atrophy and thus appear to require a rela tively intact cerebral cortex [204,298,299]. There was no association with clinical findings of depression, but psychosis predicted 22% of the variations in aggressive behavior. No relationship was iden tified between increasing severity of dementia and aggressive behavior. When it comes to individual cases, the impact of premorbid personality straits, medication, psychological environment and concomitant medical illness must be considered [301]. Patients with Parkinsonism were excluded from the study, 94 patients had delusions only, 3 had hallucinations only and 21 had both. Eightyeight patients had delusions of theft, 10 patients had delusions of being conspired against, 58 patients had misidentifica tions and delusion, 42 had delusions that someone was in the house, 11 had delusions that the house was not their own and 6 had delusions that television personalities were present in the home. Insight is a complex concept that consists of several constructs, including the ability to re-label certain mental events as pathological, the recognition of disease and the degree of compliance with treatment [179]. No relation was found between unawareness of dementia and the presence of depres sion. Weinstein et al pointed out that, despite assertions of denial in formal interviews, patients frequently exhibited awareness of their impairments in other contexts and situations [312]. Both long-lasting and reversible dialysis encephalopathies with elevations of aluminum, senile plaques and neuro fibrillary tangles have been described [314,315]. A prospective study found that the preva lence of dementia was 8% from age 35 to 40 and 55?75% above age 50 [326]. Memory failure, disorientation, a reduction of language functions, myoclonic twitchings and generalized epileptic seizures are reported. Dalton et al found a selective reduction of short-term visual retention above age 35 [329]. Lopez et al described a large kindred in which 128 individu als were identified [283]. The most common initial symptoms in the Lopera family were progressive memory failure, langu age difficulties, personality changes and, later on, gait difficulties, seizu res and myoclonus. A common feature of the affected patients was severe headache, both preceding and during the course of the disease. Other predominant symptoms were logoclonia, myoclonic twitchings, major motor seizures, psycho motor slowness with a stiff stooped gait and rapid weight loss [145,338]. The symptom pattern was explained by the consistent and severe invol vement of cortical and central gray structure and linked to chromosome 14. A fundamental question concerns the clinical implication of Lewy bodies in different cortical and subcortical regions. Whole brain semi-serial sectioning shows that the neuropathological picture is complex, varying among individual cases that sometimes exhibit a very similar clinical appearance. In addition, there are indications that the clinical picture is influenced by sensory disabilities, such as deafness and reduced vision, as well as low and labile blood pressure [344]. Cataracts were significantly associated with visual hal lucination, and no patients with normal acuity had hallucinations. Differentiating among dementias presents many difficulties, especially at an early stage, and no single available diagnostic technique can solve all of these problems. This episodic improvement in VaD, which is also found in delirious states, probably points to the potential viability of dysfunctional brain regions. Gustafson and Nilsson applied the ischemic score to clinical data from a longitudinal study of early onset dementia [303]. There are few studies of clinical differentiation based on combinations of various diagnostic rating scales. They tested the scales in conjunction with a complete neuropsychiatric examination, including an executive interview, mini-mental state examination and informant-based questionnaire. Swartz et al used a multivariate step-wise discriminant analysis and largely confirmed the validity of the clinical features [189]. Loss of personal awareness, dietary changes, perseverative behavior and reduction of speech were the most clearly differentiating items. However, there were no correlations between their performance on the frontal executive task and the tendency to produce confabulation. Various clinical publications have studied the validity of different sets of clini cal criteria vs pathological diagnostic criteria. The sensitivity of the individual clinical criteria was rather low, ranging from 35% to 56% regardless of the histopathological protocol used. That suggests that the diagnostic criteria should be recommended for research purposes, albeit with caution given that the negative predictive value in clinical practice may be relatively poor. A study by Varma et al of 56 patients with post mortem diagnoses found a high sensitivity (0. They also liked sweet food more than before, as well as drank more soft drinks, tea, coffee and alcohol. Other eating changes included tendencies to eat in a stereotyped way and order and at the same time of day. Among other oral changes were tendencies to overfill the mouth, eat non-edible foods and smoke more heavily [227]. Attitudes toward dementia Attitudes of the general public towards dementia and people with dementia have changed over time, especially the past 30 years. These reports often reflect great interest and knowledge, stressing the magnitude of the problem and the importance of new research findings, often predicting a major breakthrough in the near future. Dementia was earlier defined as progressive and irreversible with little hope for the patient and low expectations by the doctor. However, knowledge among the general population, as well as clinical experience, has changed attitudes toward the diagnosis and treatment of dementia conditions. Thus, it is important that both famous and ordinary people step forward to tell about themselves or a relative with the disease. As a result, the Swedish Alzheimer Association got off to a flying start in 1986 and the interviewee was the first chairperson. Maj Odman, another familiar voice on Swedish radio, edited a small informational publica tion in 1988 entitled ?A neglected national disease. The lack of information on dementias in earlier standard Swedish encyclopedias is surprising. General attitudes toward dementia are changing, although not as rapidly as had been expected. Only a minority of the estimated 25 000 Swedes who develop dementia each year are properly examined and diagnosed. A more likely expla nation is skepticism about the benefits of early diagnosis and drug treat ment [371]. Resources and principles for clinical diagnosis of dementia vary widely within Sweden, even when comparing neighboring health. Hopefully, such inequalities reflect ignorance and lack of training rather than unfavorable attitudes toward dementia patients. That is probably due to growing aware ness that people, both they themselves and their relatives, run a relati vely high risk of developing the disease. Several studies have shown the difficulty and ambivalence that doctors face about disclosing a dementia diagnosis to patients and families.
Buy sarafem from india
This situation went on for a while until I was suddenly I became depressed and anxious and couldn’t leave the admitted to hospital with a suspected stroke in 2016 womens health nurse practitioner generic sarafem 10mg on-line. I rang the Society and they I decided to get involved in the programme Time came to see me at home and I started a ‘Living Well with for Dementia because of my own, not very good, Dementia’ group, and this felt like a life line to me. I felt that it was a good opportunity to raise awareness about During this time, I lost my job, and I felt that this was dementia, by telling people how it is for people living with managed very badly. During this time I that if I can raise awareness and help even one person had been recovering from my stroke, struggling with my to avoid what I have been through then it would be memory and my mood, due to receiving my dementia worthwhile. I decided that I wanted to go back to work, but my employers said that they were not ready for My partner and I have been seeing Occupational me to return. They suggested a phased return, but I Therapy and Physiotherapy students as part of Time was not given any support, even when I struggled to for Dementia. I have been really keen that students get remember how to log onto my computer on my frst this exposure to dementia because it can be a hidden day. They were unable to fnd me another position and disability you cannot see that people have dementia started disciplinary procedures as I was struggling to by just looking at them. I have really enjoyed doing the do my work, even though there was no support and no programme, the students are lovely. I felt that people affected by dementia, and this information comes from couldn’t see or understand my dementia, that I wasn’t the mouth of person with dementia, and their carer and believed and that I was almost having to prove that I had this feels like a much better way for them to be learning. I was put in touch with an Early Onset Dementia service in the local hospital which was a specialist team, which was very good, with lots of activities tailored to younger people. I also began helping out with the Alzheimer’s Society, and felt valued for contributing and being involved. I began to struggle living alone, and I decided that I would relocate to live with my partner. I felt that they were scared of dementia, because my father had the condition and had been in a very bad way towards the end of his life, and therefore they held a very negative outlook about it. I felt also that as well as my family, many of friends didn’t understand the condition, and I felt that they avoided me, and stopped keeping in touch. Since I moved to live with my partner, I have struggled to receive specialist help or advice, for example obtaining a doctor’s opinion annually on whether I can continue driving. She has described me as a ‘diffcult’ case, as I don’t neatly ft into the 10 minutes appointment slot. However, living with my partner has made a great difference and she is able to support me, as has doing voluntary work at a local hospice, where having a diagnosis of dementia is not held again me. I have also been very involved in working with the Alzheimer’s Society, more recently becoming a Dementia Ambassador, as well as the Time for Dementia programme. This means enhancing the people with dementia along with their carers; and the education they receive in training. This current way of learning rarely enables Due to the initial success of Time for Dementia as students to understand and challenge stigma, or to indicated by preliminary data from its integral mixed experience and create a person-centred approach to methods evaluation, in 2017, the programme was their care, or to build the compassion and understanding widened to include a broader range of undergraduate needed to help those affected by dementia. Seeing healthcare training programmes including Allied Health people with dementia only as patients and in acute Professional. Occupational Therapy, Speech and settings can also build in attitudes towards and beliefs Language Therapy, Physiotherapy and Radiography) about dementia that are negative and that are not courses at the University of Brighton, University of appropriately optimistic about the possibility of living well Greenwich, and Canterbury Christ Church University. Emerging data from the evaluation have shown improvements in dementia knowledge and attitudes in What is Time for Dementia? These include the development of empathy Time for Dementia is an innovative undergraduate and compassion. Feedback from students who participated in the the purpose of Time for Dementia is to enhance programme has identifed four key themes: (a) Insight undergraduate learning about dementia specifcally, and and understanding, (b) Challenging attitudes and stigma, more generally about older people’s health, long-term (c) Relational learning, and (d) Enhanced dementia conditions, and the role of families in care. Students have identifed that their original perceptions of dementia had changed throughout Along with supporting workshops and refective the visits. Because Therapy and Physiotherapy students as part of Time you know, in, like, films and stuff, dementia is, like, for Dementia. I have been really keen that students get so stereotyped, like, it’s not really like that at all” this exposure to dementia, because it can be a hidden Paramedic student disability and therefore unseen, as you cannot see that people have dementia by just looking at them. I have Students also reported that the programme has really enjoyed doing the programme, the students are helped them to recognise that people can live well with lovely. They come to our house, to our environment and dementia; that people can be well supported by family this feels so much better. They are able to hear how or services and cope well with the condition, that not my partner and I have been affected by dementia, and everyone with dementia is isolated and struggling, and this information comes from the mouth of person with that many people with dementia still fnd joy in everyday dementia and their carer and this feel a much better way life. I thought that they will Newly qualifed nurse and doctors not enjoy a good quality of life. My experience of the Time for Dementia programme has informed my practice as a junior doctor, “It’s definitely made me more interested in working with when I meet patients with a diagnosis of dementia people that have dementia rather than not. I think I was a and their families I have a much greater insight and little bit scared by elderly medicine and people that have understanding of the potential struggles that the dementia and cognitive deficits before this and now it’s individual and their loved ones are going through. Notably, and challenge misconceptions held by other members students were able to develop an understanding of of the multidisciplinary team towards their understanding the importance of ‘being’ (engaging with the person) of dementia, sometimes often bleak and stereotypical rather than just ‘doing’ (performing tasks) in practice perceptions of what living with dementia really means. I which contributed to how they saw themselves as future also feel more competent in supporting families through nurses. Adult nursing students reported that that they pre diagnosis, diagnosis and advanced care planning could be active in their contribution to care and serve as in dementia. Time for Dementia has also instilled in me change agents in transforming dementia care. Remembering that people aren’t their diagnosis of Visits have helped me to reframe dementia focus on dementia and have other health conditions inclusive and the person more and what is important to them. Dr Zoe Cashin, junior doctor in practice often don’t know how to care for dementia, It is nearly four am and I have been bleeped to see a many just try and ignore it. The helps to reduce stigmagives an opportunity to slowly patient is a 69 years old lady with a background of face our misconceptions and gives the next generation dementia and Huntington’s disease. She is being treated of healthcare professionals a better understanding of for sepsis secondary to urinary tract infection. I do a quick assessment head to toe Person with dementia account and I am not clinically worried about her, but I can sense I decided to get involved in Time for Dementia because that she is scared. I hold her hand tightly to reassure of my own not very good experiences with health care her that she is safe here. I felt that it was a good opportunity to year, I have not felt hesitant to approach patients with raise awareness about dementia, by telling people how dementia. If the data continue to be positive, bonds never goes away and needs to be promoted and the next phase should be to roll it out in other health supported at all stages of the dementia journey. There is certainly no lack of people with dementia or family members Unfortunately, there is still stigma around dementia and who are willing to participate. It appears that this is one we clinicians cannot help but to find ourselves focusing small, relatively simple thing that can be done that is on presenting complaints but not the person inside. Having little experience with dementia prior to starting my degree, the Time for Dementia programme gave me an insight of how families and patients with dementia live. Working in the community I visit a lot of people who References are on their own, and many of these have dementia. Previously, I visited a patient who had dementia, but 1 Alzheimer’s Disease International. World Alzheimer Report 2016: Improving healthcare for people living with dementia: Coverage, unfortunately was not able to communicate verbally. Time for development of the Time for Dementia programme’ International Dementia highlighted not only how important holistic Journal of Geriatric Psychiatry 32: 68-75. Integrating dementia care into undergraduate nurse curricula London: Nursing Times Online: It has also taught me to be more ‘Time for Dementia: an innovation in education’ Journal of Paramedic patient and understanding, which I now use in my daily Practice 9(11). Conclusions ‘Involving people with dementia and their carers in dementia education for undergraduate healthcare professionals: a qualitative the defnitive evaluation of the programme is not study of motivation to participate and experience’ International yet completed. The testimony of student participants is that it helps students to develop appropriately positive attitudes, understanding and optimism at how well people can live with dementia. The special ingredient in Time for Dementia is that it places the people with dementia and their families as the mentors and teachers of our students. They teach what is possible in dementia by sharing their experiences of life and of health care systems both positive and negative.