Hydrea
Cheap hydrea
Baseline ultrasonography for elevated lesions Ophthalmic tumor review Shields 23 23 c nioxin scalp treatment purchase generic hydrea on-line. Small, circumscribed tumor: can be resected locally Ophthalmic tumor review Shields 31 31 3. Adenoma and adenocarcinoma may be clinical indistinguishable Ophthalmic tumor review Shields 34 34 2. Stages correlate well with prognosis for eye salvage Ophthalmic tumor review Shields 39 39 2. Acquired vasoproliferative tumor of fundus Ophthalmic tumor review Shields 41 41 1. Gray-yellow sessile lesion in nerve fiber layer Ophthalmic tumor review Shields 42 42 2. Usually diffuse or irregular orbital mass Ophthalmic tumor review Shields 49 49 b. About 70% associated with neurofibromatosis Ophthalmic tumor review Shields 50 50 4. Well circumscribed benign tumor of optic nerve 2 Composed of compact well-differentiated fibrillary astrocytes 3. Infiltration of affected tissues by chronic inflammatory cells (mostly lymphocytes) 2. Superonasal or nasal fluctuant subcutaneous mass Ophthalmic tumor review Shields 55 55 c. Arises from Schwann cells of ciliary nerves Ophthalmic tumor review Shields 56 56 3. Radiotherapy for non-resectable lesions Ophthalmic tumor review Shields 58 58 7. Malignant epithelial tumors (Adenoid cystic carcinoma, pleomorphic adenocarcinoma, etc) Ophthalmic tumor review Shields 59 59 1. Look for conjunctival salmon patch and uveal infiltration Ophthalmic tumor review Shields 60 60 3. Most of the specific tumors discussed earlier under eyelids, conjunctival and intraocular sections b. An example is the conjunctival telangiectasia of ataxia telangiectasia (Louis-Barr). Most are now recognized to be due to recessive tumor suppresser gene c Some have no hereditary pattern (Sturge-Weber and Wyburn-Mason) 4. Central Nervous System Features (Mainly in type 2) Ophthalmic tumor review Shields 65 65 a. Cornea: Occasional prominent corneal nerves (More common in multiple endocrine neoplasia syndromes d. Other cutaneous hemangiomas (May overlap the Klippel-Trenaunay Weber syndrome) 3. Central Nervous System Features a Racemose hemangioma in midbrain b Can also affect pterygoid fossa, mandible and maxilla 4. These laws required hospitals, radiation therapy centers, and in-state and out-of-state cancer diagnostic laboratories (that provide services to Maryland physicians) to electronically report all cancer cases diagnosed and/or treated in Maryland, beginning on July 1, 1993. C Myelodysplastic syndrome with 5q deletion (M-9986); D469 Myelodysplastic syndrome, unspecified (M-9975); D471 Myelofibrosis with myeloid metaplasia (primary myelofibrosis) (M-9961); D47. Extent of the disease by the end of the first hospitalization using a standard nomenclature specified by the Secretary; and 4. Extent of the disease within 4 months of diagnosis using a standard nomenclature specified by the Secretary if the information is available to the reporting facility and the reporting facility has a tumor registry; (iii) Facility and other provider identification information; and (iv) Other requirements as considered necessary by the Secretary. See Appendix 2 for a list of the fields required for reporting by type of facility/reporter. A cancer report should be submitted for each reportable primary tumor, independent of whether the tumor was microscopically confirmed, so clinically diagnosed tumors without pathologic or cytological confirmation are reportable. In the process of interpreting the clinical or pathologic diagnosis formulated by a medical practitioner, registrars should use the Ambiguous Terminology rules. The following ambiguous terms are considered diagnostic of cancer and must be reported: apparent(ly) malignant appearing appears most likely comparable with presumed compatible with probable consistent with suspect(ed) favors suspicious (for) typical of Example: the inpatient discharge summary documents that the patient had a chest X-ray consistent with a carcinoma of the right upper lobe. Are there some tumors that may not be reported based of the Class of Case definitions All reporting facilities except for laboratories and physician offices may not transmit reports with the Class of Case of 32, 33, 40, 41, 42, 43. Laboratories may not transmit reports with the Class of Case of 20, 21, 22, 32, 33, 40, 41, 42. Physician offices may not transmit reports with the Class of Case of 32, 33, and 43. In addition, physician offices may not transmit cancer reports for cases that had been previously reported by any reporter as a Class of Case 00, 10, 11, 12, 13, 14, 20, 21, 22. Appendix 2 provides the exact list of fields required for each type of reporting facility. Appendix 5 provides specific instructions on how to format and upload a disease index. Information provided to a cancer control agency in another state Notwithstanding any other provision of law, the Department may provide patient-identifying information for patients treated in this State for cancer to a cancer control agency in another state if: (1) the patient is a resident of the other state; (2) the Department determines that the agency will preserve the confidentiality of the information; and (3) the other state has the authority to provide equivalent information on Maryland residents to this State. Extent of the disease within 2 months of diagnosis if the information is available to the reporting facility and the reporting facility has a tumor registry; and (iii) Facility and other provider identification information. Submit a cancer report to the Secretary, on the form that the Secretary provides or in a computerized file; 2. Make available to the Secretary, or an agent of the Secretary, at the facility the information necessary to compile a cancer report; or 3. Enter into an agreement with a hospital or other facility or agency that agrees to report to the Maryland Cancer Registry to act as the reporting source for a cancer or central nervous system tumor patient who has been referred to or from that facility, or reported to that agency with regard to cancer or central nervous system tumor screening, diagnosis, or treatment; and (ii) Effective July 1, 1993, submit a cancer report in a computerized file on a quarterly basis to the Secretary, or an agent of the Secretary, for all patients initially diagnosed, treated, or admitted to a facility for cancer or a central nervous system tumor during that calendar quarter. This chapter establishes a cancer registry within the Department, defines key terms, details the information to be contained in a cancer report, and specifies requirements of reporting facilities, nursing facilities, assisted living programs, and general hospice care programs. In addition, this chapter identifies requestors authorized to receive confidential data, allows a fee to be charged for data reports, and incorporates by reference the Maryland Cancer Registry Data Use Manual and Procedures (July 2016). The Maryland Cancer Registry Data Use Manual and Procedures (Maryland Department of Health, July 2016) is incorporated by reference. Research that will further the cancer control goals of the State is research whose protocols have been reviewed by Department staff who have found that the research will: (1) Advance scientific knowledge or advance knowledge of clinical practice related to cancer; (2) Have approaches, aims, and methods that will allow the researcher to perform descriptive analyses or test hypotheses; (3) Have one or more investigators who have training and experience with the approaches and methods; and (4) Be conducted in a scientific environment likely to contribute to the success of the research. Information on the industrial or occupational history of an individual with cancer, to the extent such information is available; C. Relevant information on the: (1) Initial diagnosis, including the date of the diagnosis; (2) Initial treatment; (3) Extent of the disease by the end of the first hospitalization; and (4) Extent of the disease within 2 months of diagnosis, if the information is available to the reporting facility, nursing facility, assisted living program, or general hospice care program; D. A nursing facility, an assisted living program, or general hospice care program shall submit a cancer report containing information that is under the control of the facility to the Secretary if the Secretary requests a cancer report on a patient who has been a resident of the nursing facility, assisted living program, or general hospice care program. The Secretary may release confidential information, subject to: (1) A determination by the Secretary that a recipient of the information disclosed will maintain the confidentiality of the disclosed information; and (2) An agreement signed by the Secretary and by the recipient of the confidential information that the recipient of the information will maintain the confidentiality of the disclosed information. A reporting facility that in good faith submits a cancer report to the Secretary is not liable in any cause of action arising from the submission of the cancer report to the Secretary. The Secretary shall release cancer data in accordance with the procedures outlined in the Maryland Cancer Registry Data Use Manual and Procedures (July 2016). To assure compliance by a reporting facility, nursing facility, assisted living program, or general hospice care program with Regulation. Nothing in this chapter is intended to limit or otherwise restrict the Secretary from obtaining cancer report information on Maryland residents from sources located either inside or outside the State. If cancer abstraction software generates text automatically from codes, the text cannot be utilized to check coded values.
Buy hydrea 500 mg lowest price
Wherever possible medications used for migraines discount hydrea 500 mg, impairment of function should be reported in terms of objective tests or findings rather than as opinion or conjecture. Where an impairment involves an upper extremity, left or right handedness 15-6 Disposition of Problem Cases should be specified. Sufficient information for proper assessment of overall disability or func tional impairment must be presented. In cases referred to the Physical Evaluation Board, the report must contain information on all rateable conditions, even if some do not represent func tional impairment or lead to unfitness in and of themselves. It is especially important that conjecture regarding disability ratings by members of the Medical Board to the patient or his or her family be avoided. If he or she chooses to accept it, the paperwork is passed to the Physical Review Council and the Judge Advocate Generals office for review before approval by the Secretary of the Navy. Regardless, the member may present testimony from other military medical consultants or be represented by military attorneys at no cost, or he or she may retain civilian consultants and civilian attorneys at his or her own expense. If he or she remains dissatisfied, appeal is again possible, either with a full and fair or prima facie hearing, before the Physical Disability Review Board. The recommendation of this Board, after review by the Judge Advocate Generals office, is then passed to the office of the Secretary of the Navy for a decision. The patient has no formal appeal mechanism at this point, but every effort will have been made to ensure fair and impartial treatment. If the outcome is that the member is not fit for duty and that the disability rating is less than 10 15-7 U. Naval Flight Surgeons Manual percent, a separation will ensue which will terminate the members relationship with the military without compensation (unless entitlement to retirement benefits has been earned by longevity). If it is determined that the patient is not fit for continued service and that the disability rating is more than 10 percent and less than 30 percent, he or she will be separated with a lump sum severence payment, the amount of which is determined by the members longevity, rate or rank, and the actual percentage of disability established. This terminates the members relationship with the military; no other benefits will be accorded unless the member had already served on ac tive duty for a sufficient period to have established eligibility for retirement. The report of this review is essentially another Medical Board, and it should document clearly the difficulties and successes he or she has experienced in adapting to civilian life. Should the member choose not to return to active duty, the disability compensation and all other benefits would cease and he or she would be separated. These are established by multiplying the current monthly base pay for the rate or rank the member had achieved when medically retired by the percentage of disability established, with the latter limited to 75 percent; the maximum a person could receive in retirement pay after 30 years of service. For example, an O-5 with 16 years active duty who incurred a disability rated at 50 percent would receive 50 percent of the base pay for an O-5 with 16 years service. Had the disability been rated at 100 percent, he or she would receive 75 percent of the same base pay. This would be the case with many enlisted members and some junior officers with 15-8 Disposition of Problem Cases few years of active duty. In either case; medically retired members retain essentially the same rights to the use of base facilities (commissaries, exchanges, etc. All disability compensation for members continuously on active duty since before 25 September 1975 is exempted from Internal Revenue Service taxation. For those whose active ser vice commenced after that date, disability must have been incurred in combat-related cir cumstances in order to qualify for the income tax exemption. As an example, if a member reports a physical disability at the time of examination for retirement after 30 years of service and is awarded a 50 percent disability for this, he or she would receive 75 percent of the base pay of longevity, and two-thirds of this amount (50 percent of the base pay) would be exempted from Federal taxation. General Comments What has been discussed is the disposition of active duty personnel who develop an illness or sustain an injury which renders them unable to continue to function effectively. They are assured that if their ability to provide for themselves in civilian life should become compromised, they will be compensated. On the other hand, the military assumes no responsibility for inherent defects in character development which may cause an individual to be unable to function effectively, with the maturity inherently required, in a military organization. Those who cannot accept the respon sibility of military service are dealt with administratively, rather than medically, and their defi ciencies are not compensated. It should be understood clearly that whether or not a situation constitutes a problem for a member or for society is one issue: the determination of whether the same condition might compromise his or her effectiveness in military service might be entirely contrary. For example, people with certain personality disorders, people who choose to use drugs recreationally, people whose sexual preference is while not conventional not disruptive to society when conducted by mutual consent in privacy, and people who genuinely develop an irreconcilable conviction that war is wrong, might all make very positive contributions to society. Under conditions as they now prevail, however, none of these people can function effectively in military service. For that reason, an avenue to provide for their discharge by administrative means has been established. Our referring to their conditions as defects is not meant to connote a value judgement but rather to differentiate their reasons for being unable to serve from those compensable reasons which are related to diseases and injuries. Almost all officer procurement programs require either an extended period of exemplary enlisted service or selection through a competitive process which requires at least the attainment of an undergraduate degree, either of which tends to eliminate people who would have many of the kinds of difficulties to be discussed. Elsewhere in this Article, for such problems as misconduct, negligence, incompetence, disregard, and unsatisfactory or marginal performance, detachment for cause of officers is discussed, along with the additional requirements which apply in the case of detachment for cause of incumbent and prospective commanding officers and officers in charge. Throughout this Article are reaffirmations of the need for correct, comprehensive, and credible documentation in all administrative processing; also emphasized is the assurance provid ed in Navy Regulations of every members right to respond formally to any information which 15-10 Disposition of Problem Cases might be construed as adverse before such information is made a part of that members official record. The discussion begins with a listing of the formal reasons for administrative separation: 1. Expiration of Enlistment, Fulfillment of Service Obligation, Expiration of Tour of Active Service. Other designated physical or mental conditions (somnambulism, enuresis, per sonality disorders, motion sickness, allergies, excessive height, and obesity). Defective Enlistment or Induction (erroneous, defective, minority, or fraudulent). Note that many of the formal reasons listed for separation in no way imply anything negative about the member. Indeed, by far the most common reason for administrative separation of 15-12 Disposition of Problem Cases enlisted members is discharge by reason of expiration of enlistment or release to inactive duty upon completion of active obligated service. In most cases, members separated for those reasons have served effectively for the period of time for which they volunteered and now wish to exercise their prerogative of continuing their education or pursuing a different career field. On the other hand, members separated for reasons cited later in the list will have demonstrated an inability to adapt to military service and will have become a burden, instead of an asset, to their command. Individuals who lack the ability or the desire to become good sailors should be separated. Com mands must, however, devote a sincere effort to the development of those marginal members who give indication of potential for maturing into useful sailors or marines. If it becomes evident dur ing that effort that the member is not going to adjust, continued retention and further counseling would constitute a pointless drain on resources. The timely and carefully considered use of ad ministrative separation procedures can ensure staffing by individuals who will meet the standards of duty, performance, and discipline needed to accomplish the mission. The loss of training and equipment costs and related expenses, and the cost of recruiting and preparing a replacement for the member separated prior to completion of his or her obligated service should not be overlooked. But when a persons nonconformance with our standards of conduct, discipline, and perfor mance creates a high cost in terms of wasted pay, recurring administrative actions, deterioration of others morale, and compromise of mission readiness, the need for prompt administrative separation will be apparent. Less than this will invite processing delays, disapproved recommendation, violation of members rights, and litigation. An Administrative Board is required in the processing of separations of individuals who will not or cannot conform to acceptable standards of conduct, discipline, and performance, and who create high costs in terms of pay, administrative effort, degradation of morale, and substandard mission performance. It reviews the case and recommends disposition (retention, separation, or suspension of separation), assigned reason for separation, and characterization of service or description of separation. Administrative Separation is a discharge or release from active duty at or prior to the expiration of an enlistment or required period of service except any separation effected by sentence of a general or special court martial. Discharge is the complete severence from all Naval status gained by the enlistment or induction concerned. This Article continues by noting that several of the reasons for processing members for ad ministrative separation are so inconsistent with appropriate standards of conduct and perfor mance that such processing is mandatory: commission of a felonious offense, commission of a serious offense which reflects sexual perversion, homosexuality, sale or trafficking of drugs, or possession of drugs in amounts exceeding those reasonably considered to be for personal use. Pursuing a theme introduced in the preceding Article, there is an admonition (unless processing for separation is mandatory) to consider the members potential for maturation or rehabilitation which might make useful naval service possible in the future. Several factors are specifically recommended for consideration in developing the bottom-line recommendation for retention or separation. In appropriate circumstances, recommendation of suspension of separation is en couraged. With this, the separation is approved but not carried out for a specified period, not to exceed one year. The member will be retained unless carefully detailed circumstances recur; he or she will be counseled and will understand clearly that the suspension will be vacated and the separation effected promptly in the event of further problems.
Buy cheap hydrea
Our seafaring tradition includes rituals with heavy drinking treatment innovations buy genuine hydrea online, based on tenacious myths that heavy drinking signifies vigor and promotes good fellowship. Such folklore stemming from the days of the galleons has no place in modern medicine in a modem navy. It is incumbent on us in the Medical Department to dispel these myths, not only by our utterances, but more importantly by our leadership actions and by our example. Take a close look at irrational drinking customs at your command, take remedial action, and insist that your staff members act exemplarily and responsibly in their con sumption of alcohol, or avail themselves of rehabilitation. It is my desire that the Medical Depart ment take a leading role in the curtailment of irresponsible drinking in the Navy. In this revision, all efforts have been made to retain Captain Purschs unique insights and methods of dealing with alcoholism. For administrative management, the latest changes in pertinent instructions and the addition of new instructions have been includ ed. Within a variety of naval aviation communities flight operations are characterized by sustained mental and physical effort and prolonged vigilance which leads to fatigue. Fatigue is unquestionably a major consideration during many military flight operations. There are, however, many questions and unresolved issues concerning the manner in which fatigue develops, its importance in various missions, and the best way to manage it. The flight surgeon is in a key position to assist operating personnel in dealing with the multifaceted and ill-defined problem of fatigue. These investigations revealed dif ficulties in classifying fatigue, or performance decrement resulting from fatigue. These dif ficulties are related to the fact that the word has no specific scientific meaning and does not repre sent a distinct clinical entity. Instead, fatigue refers to a group of phenomena associated with impairment or loss of efficiency and skill. As a complaint it probably indicates sleep deficit, disruption, or deprivation associated with prolonged periods of work, amidst the multiple opera tional stresses of flight. It involves a subjective appreciation of tiredness, momentary lapses of at tention, and possibly impaired psychomotor performance. In view of the many operational stresses of flight, it is probable that all of them induce fatigue to some degree. For the flight surgeon, practicing operational medicine, fatigue may be considered as a state of decreased performance resulting from an accumulation of the inherent stresses of military aviation. Naval Plight Surgeons Manual the flight surgeon involved with military operations must be intimately familiar with each of the stresses that aircrew may encounter in flight. A typical list of the stresses which aircrew may encounter includes the following: 1. Enforced sitting posture and restriction of exercise during the long hours of flight. Alterations in nutrition and fluid requirements as well as available sources of food and li quids. Hypoxic environments, atmospheric pressure changes, humidity and temperature dif ferences. The effects of drugs such as caffeine, alcohol, antihistamines, and antiemetics, etc. Problems with the excretion of waste, bladder distention, constipation, diarrhea, and gastrointestinal distention due to barometric pressure changes. Middle ear problems related to barometric pressure changes such as pain of aerotitis or vertigo. Psychological stresses related to military aviation, sustained combat missions and the in terrelationships among all of these factors. Therefore, in aviation, fatigue is always a potential threat to the success of the mission and to flying safety. Sustained Operations and Fatigue the operational consequences of sustained operations (continuous performance of tasks over a prolonged period) have long been recognized. Each sustained operation will contain one or more episodes of continuous work during which time there will be no pause for rest or sleep. Three primary factors have limited the duration of continuous work during sustained operations in the past: (1) limited vision at night, (2) equipment limitations and unreliability, and (3) limited endurance of personnel. With advances in aircraft technology, sustained operations are no longer limited by aircraft reliability, weather, or darkness. The duration of continuous work episodes is now determined primarily by human en durance, which is limited by fatigue and the need for rest and sleep. The operational consequences of fatigue will play an increasingly important role in naval avia tion because of the premise that sustained operations can be a war winner. Since it may not be possible to bring additional forces to bear immediately, aircrews may have to perform at intense levels for ex tended periods with minimal or no rest or sleep. Rest will be dictated by the nature of the situation and may be fragmentary at best. Even when able to sleep, aircrews will be expected to awaken quickly to fly their missions. It is imperative that high levels of performance be maintained under severe conditions and that we learn the best way to manage the concomitant problems of fatigue. An extended time period which includes both continuous work episodes and relatively quiet periods is typical for a sustained operation. There are distinct phases such as predeployment, movement to contact enemy forces, com bat, consolidation, regrouping, and resupply. The periods of intense and continuous fighting with no chance for rest or sleep may occur many times during a sustained operation. However, there are also relatively quiet periods with opportunities for short periods of rest and sleep. The flight surgeon must be concerned with how to identify, prevent and cope with deteriorating performances, poor moods, and lowered willingness to work caused by fatigue and lack of sleep. Naval Flight Surgeons Manual He must be able to advise the operational forces when and how they will best be able to recuperate from the stress and fatigue of continuous work episodes and maintain, as an individual and as a fighting unit, combat effectiveness during a sustained operation. Sleep Deprivation Although performance depends on complex interactions between tasks, work schedule, en vironmental stresses, and the individual, it will certainly be impaired when the aviator becomes sleepy. The disruption of the sleep-wakefulness cycle with some sleep loss is likely to be a problem in all air operations which extend beyond a single day, and sleep loss is likely to intensify as the duration of the mission increases. The need for sleep (sleep deprivation) is probably the major component contributing to operational fatigue in continuous work episodes during sustained operations. Although fatigue and sleep deprivation can be defined as acute, chronic, or cumulative and correlated to some extent with biochemical aberrations, we are unable to determine objectively at what point an individual will experience a performance decrement. Difficulties in determining when fatigue and sleep loss result in impaired performance stem from the fact that laboratory performance tests may not be sensitive to the type of deficits which occur. Variables such as extensive training, high motivation, and interest can counteract some of the effects of sleep loss and fatigue. Performance decrement is not always present in all individuals and may be intermittent. However, as fatigue and sleep deprivation accumulate, symptoms will be more prevalent and last longer. When these symptoms appear in each individual depends not only on hours of wakefulness but also on tolerance to sleep loss, type of tasks to be performed, severity of physical workload, and time of work in relation to the individuals circadian rhythm. During operational conditions there is always doubt concerning the extent of sleep loss, as it is difficult to avoid very short periods of sleep. In field studies it is difficult to suppress sleep, and total loss of sleep has probably only been achieved in laboratory experiments when the elec troencephalogram has been continuously monitored. During laboratory experiments involving long periods of wakefulness, drowsiness and microsleeps readily occur. They become more fre quent as the period of wakefulness continues, and if not immediately aroused the individual will rapidly fall asleep. Therefore, sleep loss is a continuum which extends from a normal sleep wakefulness pattern to microsleeps and drowsiness and finally to total sleep loss. There is little evidence, however, that drowsiness (the transition between wakefulness and sleep) or microsleeps preserve performance in sustained wakefulness. In these early studies, most subjects functioned fairly well during restricted sleep schedules, but many of the tests used did not reflect the complex tasks that are required in tactical aviation during sustained operations. Because many of the studies estimating performance decrement in sustained operations included a mixture of more or less sensitive cognitive tasks, intermittent testing, and nondemanding in terest intervals, their estimates of expected performance degradation were felt to be conservative.

Order online hydrea
For example medications rapid atrial fibrillation buy generic hydrea 500mg on line, an applicant with a history of bleeding ulcer may be required to have the physician submit followup reports every 6-months for 1 year following initial certification. The prophylactic use of medications including simple antacids, H-2 inhibitors or blockers, proton pump inhibitors, and/or sucralfates may not be disqualifying, if free from side effects. An applicant with a history of gastric resection for ulcer may be favorably considered if free of sequela. Mental disorders, as well as the medications used for treatment, may produce symptoms or behavior that would make an airman unsafe to perform pilot duties. Records must be in sufficient detail to permit a clear evaluation of the nature and extent of any previous mental disorders. Opinions regarding clinically or aeromedically significant findings and the 307 Guide for Aviation Medical Examiners potential impact on aviation safety must be consistent with the Federal Aviation Regulations. Due to the differences in training and areas of expertise, separate evaluations and reports are required from both a qualified psychiatrist and a qualified clinical psychologist for determining an airmans medical qualifications. Psychiatric evaluations must be conducted by a qualified psychiatrist who is board-certified by the American Board of Psychiatry and Neurology or the American Board of Osteopathic Neurology and Psychiatry. The psychiatrists comprehensive and detailed report, as noted above, plus copies of supporting documentation. Clinical psychological evaluations must be conducted by a clinical psychologist who possesses a doctoral degree (Ph. Using a psychologist without this background may limit the usefulness of the report. Opinions regarding clinically or aeromedically significant findings and the 310 Guide for Aviation Medical Examiners potential impact on aviation safety must be consistent with the Federal Aviation Regulations. Additional Helpful Information: Will additional evaluations or testing be required in the future If eligible for unrestricted medical certification, no additional evaluations would be required. The letter authorizing special issuance will outline the specific evaluations or testing required. Requirements for providing records to the neuropsychologist, conducting the evaluation, and submitting reports are the same as noted above for the clinical psychologist. The neuropsychologists report as specified in the portal, plus: Copies of all computer score reports; and An appended score summary sheet that includes all scores for all tests administered. Follow the guidance in the Substances of Dependence/Abuse (Drugs and Alcohol) section in this document. Current status report including: Detailed family history of thromboembolic disease; Neoplastic workup, if clinically indicated; Blood clotting disorders. Specifically, sleep apneas are characterized by abnormal respiration during sleep. All sleep disorders are also potentially medically disqualifying if left untreated. Target goal should show use for at least 75% of sleep periods and an average minimum of 6 hours use per sleep period. Once Dental Devices with recording / monitoring capability are available, reports must be submitted. How am I supposed to determine if an airman is high risk enough to send for a sleep evaluation However, it may be useful to document the rationale for triage decisions, especially for Group/Box 2, 5, and 6. Guide for Aviation Medical Examiners 8. Issue a regular (not time limited) certificate, if the airman is otherwise qualified. Does he have to wait for a time-limited certificate before he can return to flight duties At that point, he/she will have to comply with the new documentation requirements. Guide for Aviation Medical Examiners 17. If I give the airman Specification Sheet A or B and he does not submit the required evaluation within 90 days and after the 30 day extension (if requested), what will happen What if the airman is high risk and has had a previous sleep study that was positive, but not one of the approved tests If the airman is determined to be Group/Box 5 or 6, he/she will need a sleep evaluation. Rarely or never Dont know Guide for Aviation Medical Examiners Scoring Berlin Questionnaire the questionnaire consists of 3 categories related to the risk of having sleep apnea. Patients can be classified into High Risk or Low Risk based on their responses to the individual items and their overall scores in the symptom categories. Categories and Scoring: Category 1: Items 1, 2, 3, 4, and 5; Item 1: if Yes, assign 1 point Item 2: if c or d is the response, assign 1 point Item 3: if a or b is the response, assign 1 point Item 4: if a is the response, assign 1 point Item 5: if a or b is the response, assign 2 points Add points. Item 6: if a or b is the response, assign 1 point Item 7: if a or b is the response, assign 1 point Item 8: if a is the response, assign 1 point Add points. However, it soon became clear that some people did not answer all the questions, for whatever reason. It is not possible to interpolate answers, and hence item-scores, for individual items. Snoring Do you snore loudly (louder than talking or loud enough to be heard through closed doors) There are numerous conditions that require the chronic use of medications that do not compromise aviation safety and, therefore, are permissible. Airmen who develop short-term, self-limited illnesses are best advised to avoid performing aviation duties while medications are used. Aeromedical decision-making includes an analysis of the underlying disease or condition and treatment. The underlying disease has an equal and often greater influence upon the determination of aeromedical certification. It is unlikely that a source document could be developed and understood by airmen when considering the underlying medical condition(s), drug interactions, medication dosages, and the sheer volume of medications that need to be considered. Maintaining a published a list of "acceptable" medications is labor intensive and, in the final analysis, only partially answers the certification question and does not contribute to aviation safety. The lists of medications in this section are not meant to be all-inclusive or comprehensive, but rather address the most common concerns. Guide for Aviation Medical Examiners Do Not Issue. New antibiotics, lipid-lowering drugs, and antihypertensive medications may be considered earlier than one year. Airmen should not fly while using any of the medications in the Do Not Issue section above or while using any of the medications or classes/groups of medications listed below without an acceptable wait time after the last dose. All of these medications may cause sedation (drowsiness) and impair cognitive function, seriously degrading pilot performance. This impairment can occur even when the individual feels alert and is apparently functioning normally in other words, the airman can be unaware of impair. For example, there is a 30-hour wait time for a medication that is taken every 4 to 6 hours (5 times 6) Label warnings. Such medications can cause impairment even when the airman feels alert and unimpaired (see unaware of impair above). Medications such as loratadine, desloratadine, and fexofenadine may be used while flying, if symptoms are controlled without adverse side effects after an adequate initial trial period. This includes but is not limited to morphine, codeine, oxycodone (Percodan, Oxycontin), and hydrocodone (Lortab, Vicodin, etc. This includes all drugs used as an aid to outpatient surgical or dental procedures. The wait time after diphenhydramine is 60 hours (based on maximum pharmacologic half-life). Guide for Aviation Medical Examiners the list of medications referenced below provides aeromedical guidance about specific medications or classes of pharmaceutical preparations and is applied by using sound aeromedical clinical judgment. For applicants using oral isotretinoin (Accutane), there is a mandatory 2-week waiting period after starting isotretinoin prior to consideration.
Buy hydrea 500mg with amex
The juvenile form usu cellular marrow inltration as T1-hypointense and T2-isointense ally involves the musculoskeletal system medicine vials discount hydrea 500 mg visa. In younger mass or masses (T1-isointense to hypointense, T2-isointense to patients, it may be difficult to distinguish tumor inltration of hypointense or hyperintense, with gadolinium enhancement, marrow from the hematopoietically active red marrow (also T1 with use of fat-suppression techniques), that extends along tissue hypointense, T2-isointense to hyperintense, and enhancing). Conversion to yellow marrow (increased fat content, therefore T1-hyperintense) occurs with increasing age as well as with the Other Malignant Tumors of Mesenchymal Origin myelosuppressive effects of radiotherapy and chemotherapy. Osteosarcoma is an osteoid-forming neoplasm and the most com Marrow inltration may then be more readily detected until there mon primary bone neoplasm of childhood. Subtypes include is red marrow rebound after therapeutic response (including after osteoblastic, chondroblastic, telangiectatic, and broblastic. A mottled marrow pattern may Spinal involvement is infrequent and may be metastatic. Fat-suppres some cases it may be radiation-induced or may arise from an sion T2-weighted techniques. Treatment includes surgery, chemotherapy, and ra markedly enhancing masses that may be associated with bone diotherapy. Treatment includes umn as a mass, or may represent lymphatic or hematogenous me surgery and radiotherapy. Tumors of Neural Crest Origin Ewing sarcoma arises from the primitive reticulum stem cell the spinal tumors of neural crest origin include neuroblastoma, (bone marrow origin) and is a common tumor of childhood. It is composed of neuroblasts and arises within the sympathetic nervous system. Non-uniform intensities may be related to calcication, hemorrhage, edema, and necrosis. Its behavior may be similar to that of neuroblastoma, including metastases and spinal canal extension. Images show a T2-weighted hyperintense and enhancing neoplasms of primitive neuroepithelial origin. Imaging ndings posterior mediastinal and paraspinal mass (anterior long arrows), intraspi are similar to those for other round cell tumors, including soft nal extension (posterior long arrows), and marrow involvement (vertical tissue mass, bone destruction, and calcication (as discussed arrows). Seeding may rarely occur with astrocyto ma, choroid plexus tumors, lymphoma, leukemia, retinoblastoma, or rhabdomyosarcoma. Hemor rhagic or enhancing postoperative subdural or subarachnoid collections, and inammatory or infectious processes may mimic neoplastic seeding. The majority of the intramedullary tumors in childhood are astrocytomas and gangliogliomas, and fewer are ependymomas. Cervicothoracic spinal cord astrocytoma on sagittal T2 Gangliogliomas and ependymomas are often more circumscribed. It may be circumscribed or may inltrate the conus medul nonenhancing cystic component (short arrows). Philadelphia, Lippincott-Raven, fracture), which may be associated with a paraspinal or epidural 2005. There may be diffuse homogenous or inhomogeneous mar Blaser S I, Illner A, Castillo M, et al: Peds Neuro: 100 Top Diagnoses. Intradural (Extramedullary) Tumors Tortori-Donati P, Rossi A: Pediatric Neuroradiology. Intradural tumors arise within the dural sac and outside the spinal van der Knaap M S, Valk J: Magnetic Resonance of Myelination and Myelin cord. Louis, Mosby-Year developmental tumors (discussed earlier), and meningeal tumors Book, 1992. Schwannomas often occur sporadically in Zimmerman R A, Gibby W A, Carmody R F (eds): Neuroimaging: Clinical and childhood. Neuroimaging ment is common, including epidural foraminal and intraspinal Clin North Am 1999;9(1). According to the psychosocial perspective, the social worker should: (A) have her tell you about the issues affecting her life (B) begin training behavioral techniques (C) provide a referral to a psychologist for testing (D) refer to a marriage and family therapist the correct answer is A Always take time to listen and explore your clients needs and feelings. Often, you may be the only person in their life who will listen and hear their feelings, thoughts, ideas, etc. It is generally considered a specialty and should not be used by anyone without the proper training. As a new clinical social worker you find yourself being told by your supervisor you need to be more confrontational. Just because we know we should do something does not mean we will act in the appropriate manner. You demonstrate an accurate understanding by reflective listening (telling the client what you think you heard them say) and by asking questions for clarification. This is the ultimate goal of many therapies and an end result you should always look to achieve. The primary function of your unit is to educate sexually active individuals about the disease and to help them understand the importance of testing, life-style changes and treatment if necessary. The goal of secondary prevention is to identify and detect disease in its earliest stages, before noticeable symptoms develop, when it is most likely to be treated successfully. With early detection and diagnosis, it may be possible to cure a disease, slow its progression, prevent or minimize complications, and limit disability. Crisis intervention, may be provided at the Primary, Secondary or even Tertiary levels of intervention. Tertiary prevention programs aim to improve the quality of life for people with various diseases by limiting complications and disabilities, reducing the severity and progression of disease, and providing rehabilitation (therapy to restore functionality and self-sufficiency). Unlike primary and secondary prevention, tertiary prevention involves actual treatment for the disease and is conducted primarily by health care practitioners, rather than public health agencies. The first category includes actions to protect against disease and disability, such as getting immunizations, ensuring the supply of safe drinking water, applying dental sealants to prevent tooth decay, and guarding against accidents. General action to promote health is the other category of primary prevention measures. Health promotion includes the basic activities of a healthy lifestyle: good nutrition and hygiene, adequate exercise and rest, and avoidance of environmental and health risks. B) the need for the client to accept the services provided because they are identified as necessary by the social work case manager. D) the need for the social worker to develop and maintain a therapeutic relationship with the client. The correct answer is B Social Work always allows the client the right of self-determination. Just because you (the professional social worker) believes the client needs a certain services does not obligate the client to accept or utilize that service. Like all methods of social work practice, case management rests on a foundation of professional training, values, knowledge, theory, and skills used in the service of attaining goals that are established in conjunction with the client and the clients family, when appropriate. This is what makes social work different (and a more powerful intervention than other clinical services). Clients will often have needs which they may consider trivial or embarrassing and will not allow these needs to be known to the social work case manager until a bond of trust and empathy is created. You are sitting in a case staffing meeting at your agency while several other social workers are discussing their new cases and receiving feedback and suggestions. A) A 17 year-old son who needs to separate psychologically from his family B) A couple with two children that has decided to divorce. C) A separated couple with two children, one child in the family has an eating disorder D) An enmeshed family, where improvement in one member is likely to cause distress in the other members the correct answer is A this is a situation where one member of a structural unit needs to leave (or be pushed out) of the structural unit. Individual therapy and crisis intervention during the separation are the best possible therapy choices. Family therapy may be appropriate after the separation and after a set period of time has passed, in order to explore the new role. The family should explore its new roles and the expectations, both stated and implied, which are going to change in the new structure. Structural Family Therapy (Salvador Minuchin) would argue that only by restructuring all the roles in the family, can you help the individual with an eating disorder. When one family members role begins to change because of growing awareness in therapy, the entire system will begin to destabilize and cause other family members stress until it again reaches a state of equilibrium.
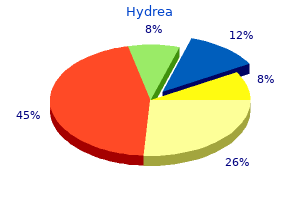
Buy hydrea 500mg online
Not Acceptable Cellular elements of interest are not visualized compromising interpretation of the stain medicine hat news order genuine hydrea line. Table 2: Background Acceptability Criteria Interpretation Microscope Observation Acceptable Non-specifc staining that is not obtrusive to interpretation of specifc staining. Not Acceptable Non-specifc staining that is obtrusive to interpretation of specifc staining. The control tissue (an index case) should be applied and the instrument functioned properly. The positive tissue a fresh autopsy, biopsy, surgical specimen prepared and fxed as control should be used only to monitor performance; it should not soon as possible in a manner identical to patient specimens. A tissue section fxed or processed differently from the test human term placental tissue, which shows moderate to strong specimen can be used as a control for reagents and staining but not uniform staining of the membrane and weak to strong uniform for fxation or tissue preparation. A positive urothelial carcinoma case staining of the cytoplasm of trophoblast-lineage cells. Placental with moderate staining is more suitable for quality control than one stromal tissue and vasculature can be used for assessment of any that stains strongly; it can be used to detect minor levels of reagent background staining. Not Acceptable No to weak uniform membrane staining of trophoblast lineage cells and/or specifc staining within placental stromal and vascular tissue. Specifcally, this guide highlights an expression level of greater than or equal to 25% of tumor cells with membrane staining or of tumor-associated immune cells with staining. Interpretation of urothelial carcinoma cases stained with the Assay is based on the criteria noted in the table below. Images of various expression level staining patterns are provided in the subsequent sections. H&E slide is reviewed for viable tumor, tumor-associated immune cells and tumor area. Tumor area encompasses the tumor proper, associated desmoplastic stroma and immune cells infltrating the tumor and contained within the desmoplasia. Tumor associated immune cells include those present within the tumor reactive stroma, between the tumor islands and those invading the tumor proper. If a raw percentage falls between a decile or quartile, standard mathematical rounding is used to score to the nearest decile or quartile. Estimate the percentage of tumor cells with partial or complete membrane staining at any intensity. Review tumor cells at 10X or 20X to evaluate for membrane staining at any intensity. Determine percentage of tumor cells with membrane staining by reviewing at 2X or 4X, if needed. Areas not considered part of the tumor diffcult to quantify the amount of staining for each component. Review case H&E to assess viable tumor with attached desmoplastic stroma containing tumor-associated immune cells. Immune Cell scoring 2:Tumor area containing tumor cells, desmoplastic stroma and tumor-associated immune cells is outlined in blue, which includes immune cell aggregates identifed by black arrows. Exclude non-neoplastic areas not involved by tumor, areas with necrotic tumor, crush and cautery artifacts. Immune Cell scoring 3:Tumor area consists of only viable areas of tumor and desmoplasia (areas outlined in blue). If tumor islands are separated by muscle or stroma, they are included as part of the tumor area if the tumor borders on both sides within a 10X feld. When viewed at higher power (10X), the stroma with tumor on both sides within a single feld of view (blue) is included in the overall tumor area. When the large bundle of fbromuscular stroma is not bordered by tumor within a single 10X feld (black), it is not included in the overall tumor area. For noninvasive urothelial carcinoma (papillary carcinoma), include the immune cells within the fbrovascular cores as well as within the immediately adjacent base of the frond/stalk. A B A B Immune Cell scoring 5:Double sided arrow (black) shows base of papillary tumor with the tumor area for this noninvasive urothelial carcinoma outlined (blue). Please refer to the associated H&E image contained within this guide, Immune Cell scoring 6. In cases where the tumor does not generate a stromal response, the tumor area is limited to the tumor nests and adjacent immune cells in direct contact with the tumor only. Immune Cell scoring 12:In this metastatic tumor to a lymph node, the tumor area containing tumor cells, desmoplastic stroma and immune cells is outlined in blue (4X). Various Occasionally in urothelial carcinoma samples endogenous staining patterns and morphologic features may make interpretation material, such as melanin pigment or hemosiderin, may obscure and quantifcation of tumor membrane staining diffcult. Some specimens may exhibit weak cytoplasmic staining of the Some challenging cases are shown. The presence of immune cells infltrating the tumor should be confrmed using the H&E slide. These cases are particularly challenging to estimate the percent of target cells with staining. For these borderline cases it may be helpful to view the case at a magnifcation that enables the entire tumor area to be assessed. A fragment-by-fragment examination approach with individual percent staining estimates followed by an overall average can help in the evaluation. Examination at higher power (20X) shows there is scattered weak tumor membrane staining. Careful examination of the tumor demonstrates cells with weak membrane expression (blue outlines) that should also be counted towards the total percentage of membrane staining. The blue outlines contain areas with discernible immune cell staining with the green outlined area having scattered punctate immune cell staining. Examination at higher power (20X) reveals tumor cells with 20% weak, delicate membranous staining. Programmed death-1 ligand 1 interacts specifcally with the B7-1 costimulatory molecule to inhibit T cell responses. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Outside border line is shown here for illustrative purposes only and does not print. Label dimensions are contained in the drawing of the label stock found on the bill of materials. Lot Number, Expiry Date, and 2D barcode are shown here for illustrative purposes only. Lot Number, Expiry Date, barcodes, and barcode-related human readable text are shown here for illustrative purposes only. Whenever this information is used in part or in whole, or when referencing it as part of a report or article, we request that acknowledgment be given to the American Board of Medical Specialties. The anesthesiologist also diagnoses and treats acute, chronic, disease, organ transplantation, or malignancies of the immune system. However, formal special pathways are available for physicians seeking Specialty training required prior to certifcation: Four years dual certifcation in Allergy/Immunology and Pediatric Pulmonology; Allergy and Immunology and Pediatric Rheumatology; and Allergy and Subspecialties Immunology and Adult Rheumatology. Additional information is available Certifcation in one of the following subspecialties requires additional from the board. Specialty training required prior to certifcation: Prior certifcation in Critical Care Medicine Internal Medicine or Pediatrics; two years in Allergy and Immunology. An anesthesiologist who specializes in Critical Care Medicine diagnoses and treats patients with critical illnesses or injuries, particularly trauma victims and patients with multiple organ dysfunction who require care over a period of hours, days, or weeks. Hospice and Palliative Medicine An anesthesiologist who specializes in Hospice and Palliative Medicine provides care to prevent and relieve the suffering experienced by patients with life-limiting illnesses. This specialist works with an interdisciplinary hospice or palliative care team to maximize quality of life while addressing the physical, psychological, social, and spiritual needs of both patient and family. Pediatric Anesthesiology An anesthesiologist who specializes in Pediatric Anesthesiology provides Colon and Rectal Surgery anesthesia for neonates, infants, children, and adolescents undergoing surgical, diagnostic, or therapeutic procedures as well as appropriate A colon and rectal surgeon diagnoses and treats various diseases of pre and post-operative care, advanced life support, and acute pain the small intestine, colon, rectum, anal canal, and perianal area including management. They treat conditions such Sleep Medicine as hemorrhoids, fssures (painful tears in the anal lining), abscesses and An anesthesiologist who specializes in Sleep Medicine has expertise fstulaes (infections located around the anus and rectum).
Buy genuine hydrea
Indicates that the patient has distant (discontinuous) metastases but distant lymph node(s) are not mentioned as an involved site Example: Use code 0 when the patient has metastasis to lung and liver but not distant lymph node(s) medications for fibromyalgia generic 500mg hydrea mastercard. In other words, use code 9 when there are known distant metastases but it is not known whether the distant metastases include distant lymph node(s). This field identifies any type of distant involvement not captured in the Mets at Diagnosis-Bone, Mets at Diagnosis-Brain, Mets at Diagnosis-Liver, Mets at Diagnosis-Lung, and Mets at Diagnosis-Distant Lymph Nodes fields. It includes involvement of other specific sites and more generalized metastases such as carcinomatosis. Use of codes: Assign the code that best describes whether the case has other metastases at diagnosis a. Indicates that the patient has distant (discontinuous) metastases but other sites are not mentioned as involved Example: Use code 0 when the patient has metastasis to lung and liver only. Includes, but not limited to , the adrenal gland, bone marrow, pleura, malignant pleural effusion, peritoneum, and skin ii. Example 1: Patient with breast cancer noted to have mets to the liver and carcinomatosis. Codes 0-7 are hierarchical; use the highest code that applies (0 is highest, 7 is lowest) 2. Definitions Active surveillance: A treatment plan that involves closely watching a patients condition but not giving any treatment unless there are changes in test results that show the condition is getting worse. Active surveillance may be used to avoid or delay the need for treatments such as radiation therapy or surgery, which can cause side effects or other problems. Cancer tissue includes primary tumor and metastatic sites where cancer tissue grows. Example: Chemotherapy and radiation therapy Deferred therapy: Closely watching a patients condition but not giving treatment unless symptoms appear or change, or there are changes in test results. Expectant management avoids problems that may be caused by treatments such as radiation or surgery. See below for detailed information on timing and treatment plan documentation requirements. Neoadjuvant therapy: Systemic therapy or radiation therapy given prior to surgery to shrink the tumor. Surgical procedure: Any surgical procedure coded in the fields Surgery of Primary Site, Scope of Regional Lymph Node Surgery, or Surgery of Other Regional or Distant Sites. Treatment: Procedures that destroy or modify primary (primary site) or secondary (metastatic) cancer tissue. It is also used when the risks of treatment are greater than the possible benefits. Use the documented first course of therapy (treatment plan) from the medical record. First course of therapy ends when the treatment plan is completed no matter how long it takes to complete the plan. Keep the refused codes even if the patient later changes his/her mind and decides to have the prescribed treatment i. Code the treatment given as first course even if the correct primary is identified later when a patient is diagnosed with an unknown primary Example: the patient is diagnosed with metastatic carcinoma, unknown primary site. Do not code treatment added to the plan when the primary site is discovered as first course. This is the start date of any type of treatment for this tumor; surgery, chemotherapy, radiation therapy, or other types of therapy. Code the date of excisional biopsy as the date therapy initiated when it is the first treatment. Code the date of a biopsy documented as incisional when further surgery reveals no residual or only microscopic residual. Example: Breast biopsy with diagnosis of infiltrating duct carcinoma; subsequent re-excision with no residual tumor noted. Code the date of admission to the hospital for inpatient or outpatient treatment when the exact date of the first treatment is unknown 6. When it is known the patient had first course therapy, but it is impossible to estimate the date d. Assign code 11 when no treatment is given during the first course, the first course is active surveillance/watchful waiting, or the initial diagnosis was at autopsy 4. Code Label Definition 0 No treatment given the patient did not receive any treatment 1 Treatment given the patient received treatment 2 Active surveillance the patient was under active surveillance or watchful waiting during the (watchful waiting) first course of treatment 9 Unknown if treatment It is unknown whether or not the patient received treatment given Coding Instructions 1. Assign code 1 when the patient receives treatment collected in any of the following fields a. Surgery date should be the same as the Date Therapy Initiated when surgery is the only treatment administered 3. Record the polypectomy date as the date of first surgical procedure when a surgical procedure to remove polyps is performed without removing the entire tumor, and a subsequent surgery is performed. Code Label Definition Blank A valid date value is provided in Date of First Surgical Procedure 10 No information No information whatsoever can be inferred 11 Not applicable No proper value is applicable in this context 12 Unknown A proper value is applicable but not known Coding Instructions 1. This data item captures the date of the most definitive surgical procedure of the primary site performed as part of the first course of therapy. Date flag fields were added beginning with diagnoses on or after 01/01/2010 as part of an initiative to standardize date fields. A surgical procedure to the primary site was done, but no information on the type of surgical procedure is provided. Use the site-specific coding scheme corresponding to the primary site or histology 3. Code the most invasive, extensive, or definitive surgery if the patient has multiple surgical procedures of the primary site even if there is no residual tumor found in the pathologic specimen from the more extensive surgery Example: Patient has a needle biopsy of prostate that is positive for adenocarcinoma. All gross disease is removed and there is only microscopic residual at the margin Note 1: Do not code an excisional biopsy when there is macroscopic residual disease. The previous procedure may have been cancer directed or non-cancer directed surgery. Assign the surgery code(s) that best represents the extent of the surgical procedure that was actually carried out when surgery is aborted. The regional lymph node surgical procedure(s) may be done to diagnose cancer, stage the disease, or as a part of the initial treatment. Code the removal of intra-organ lymph nodes in Scope of Regional Lymph Node Surgery Example: Local excision of breast cancer. Pathology identifies prostate cancer as well as the bladder cancer and 4/21 nodes positive for metastatic adenocarcinoma. The operative report lists a lymph node dissection, but no nodes were found by the pathologist 8. When mapping fails, surgeons usually perform a more extensive dissection of regional lymph nodes. When mapping fails, the surgeon usually performs a more extensive dissection of regional lymph nodes. Code 9: the status of regional lymph node evaluation should be known for surgically treated cases. Review surgically treated cases coded as 9 in Scope of Regional Lymph Node Surgery to confirm the code. The operative report will designate the surgeons planned procedure as well as a description of the procedure that was actually performed. Excisional biopsy or aspiration of regional lymph nodes for breast cancer is uncommon. Review the operative report to confirm that an axillary incision was made and a node exploration was conducted. This event occurred, but the date is unknown (for example, sentinel lymph node biopsy performed but date is unknown). Document the total number of nodes sampled during the sentinel node procedure in this data item when both sentinel and non-sentinel nodes are sampled during the sentinel node biopsy procedure; i.